Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2019, vol. 18(2), pp. 107–111 DOI: https://doi.org/10.15388/LietChirur.2019.18.12
A case report of desmoid type fibromatosis of the breast
Lina Pankratjevaitė
Chirurgijos klinika, Medicinos fakultetas, Medicinos akademija, Lietuvos sveikatos mokslų universiteto ligoninė, Eivenių g. 2, LT-50009 Kaunas, Lietuva
Department of Surgery, Faculty of Medicine, Medical Academy, Hospital of Lithuanian University of Health Sciences, Eivenių Str. 2, LT-50009 Kaunas, Lithuania
E-mail: linapankratjevaite@gmail.com
Ieva Ceslevičienė
Chirurgijos klinika, Medicinos fakultetas, Medicinos akademija, Lietuvos sveikatos mokslų universiteto ligoninė, Eivenių g. 2, LT-50009 Kaunas, Lietuva
Department of Surgery, Faculty of Medicine, Medical Academy, Hospital of Lithuanian University of Health Sciences, Eivenių Str. 2, LT-50009 Kaunas, Lithuania
Lina Poškienė
Patologinės anatomijos klinika, Medicinos akademija, Lietuvos sveikatos mokslų universiteto ligoninė, Eivenių g. 2, LT-50009 Kaunas, Lietuva
Department of Pathology, Medical Academy, Hospital of Lithuanian University of Health Sciences, Eivenių Str. 2, LT-50009 Kaunas, Lithuania
Algirdas Boguševičius
Chirurgijos klinika, Medicinos fakultetas, Medicinos akademija, Lietuvos sveikatos mokslų universiteto ligoninė, Eivenių g. 2, LT-50009 Kaunas, Lietuva
Department of Surgery, Faculty of Medicine, Medical Academy, Hospital of Lithuanian University of Health Sciences, Eivenių Str. 2, LT-50009 Kaunas, Lithuania
Abstract. Background. Desmoid type fibromatosis of the breast is a rare fibroblastic proliferative disease. It may be sporadic or associated with trauma, Gardner’s syndrome, etc. Desmoid tumour of the breast is a benign, locally aggressive disease. However, it does not metastasize. Case report. We report a case of a 65-year-old woman with right breast desmoid type fibromatosis. Conclusions. Diagnosis of breast desmoid tumour is difficult: clinically and radiologically it may mimic carcinoma. Definitive diagnosis is proved just by histopathological examination results. First choice treatment of breast fibromatosis is a radical surgical excision.
Key words: breast fibromatosis, extraabdominal desmoid tumour, rare breast disease.
Krūties desmoidas: klinikinis atvejis
Santrauka. Įvadas. Krūties desmoidinio tipo fibromatozė – retai pasitaikanti sporadinė arba su trauma, Gardnerio sindromu ar kitais susirgimais susijusi liga. Nors krūties desmoidas yra gerybinis, jam būdingas agresyvus lokalus augimas, neplintant į atokius audinius. Klinikinis atvejis. Pristatomas 65 metų pacientės, sirgusios dešinės krūties desmoidinio tipo fibromatoze, sėkmingo chirurginio gydymo klinikinis atvejis. Išvados. Krūties desmoido diagnostika sudėtinga, nes tumoras kliniškai ir radiologiškai gali imituoti karcinomą. Galutinė diagnozė patvirtinama tik patologiškai ir histologiškai ištyrus operacinę medžiagą. Pirmojo pasirinkimo gydymas – radikali ekscizija.
Reikšminiai žodžiai: krūties fibromatozė, ekstraabdominalinis desmoidas, reta krūties liga.
Received: 2019/02/28, Accepted: 2019/04/10.
Copyright © 2019 Lina Pankratjevaitė, Ieva Ceslevičienė, Lina Poškienė, Algirdas Boguševičius. Published by Vilnius University Press.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Desmoid tumour (syn. aggressive fibromatosis, nonmetastasing fibrosarcoma) is a rare benign fibroblastic proliferative disease. It can occur anywhere in the body: most common places are extremities, abdominal wall and intraabdominal cavity. Desmoid tumour is found in only 0.2% of breast tumours [1]. It may be sporadic, but also it may occur after surgical trauma, implantation of silicone breast implants or may be associated with Gardner’s syndrome [2]. Most cases of breast fibromatosis are reported in female, however it may occur in male [2, 3].
Breast desmoid tumour presents as firm, painless and movable mass [4]. Nipple, skin retraction may be seen [2, 4]. Clinically and radiologically it may mimic breast carcinoma [3]. However, conclusive diagnosis is made after histopathological examination of the lesion. Surgery, radiotherapy, chemotherapy, hormonal therapy may be used for the treatment of desmoids tumour [1, 4–6]. Radical surgical excision is the treatment of choice [5].
Case report
A 65-year-old female presented with a palpable lump in her right breast for 5 months. There was no family history of the breast cancer. Her past medical history was significant for total hysterectomy with bilateral salpingo-oophorectomy twenty years ago because of myomatous uterus and benign cysts of ovaries. She reported the onset of menarche at age 14. The patient had two deliveries.
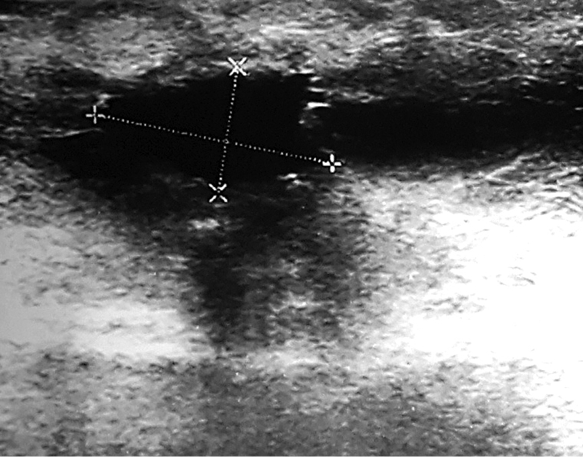
Fig. 1. The lesion was seen on ultrasound image
During physical examination a 2 cm hard, not tender, with ill-defined margins lump in the upper inner quadrant of the right breast has been found. There was no nipple retraction, discharge or skin change. A breast ultrasound showed a 1.24x0.85 cm suspicious ill-defined hypoechogenic lesion at 1 o’clock position of the right breast (Figure 1). Mammogram revealed a local hyperdense zone in the right breast (Figure 2). Histopathological examination of the tumour core biopsy material revealed desmoid type fibromatosis. The patient underwent wide local with clear margins excision of the lesion. Histopathological examination of surgical material confirmed desmoid type fibromatosis (Figure 3). Tumour was poorly demarcated, composed of spindle-shape myofibroblasts arranged in long sweeping fascicles. There was no mitotic activity. Immunohistochemical findings of the mass showed a focally positive reaction with beta-catenin, and a negative reaction for CD34, Desmin, CK. The patient did not require any adjuvant treatment. There was no recurrence after two years of follow-up.
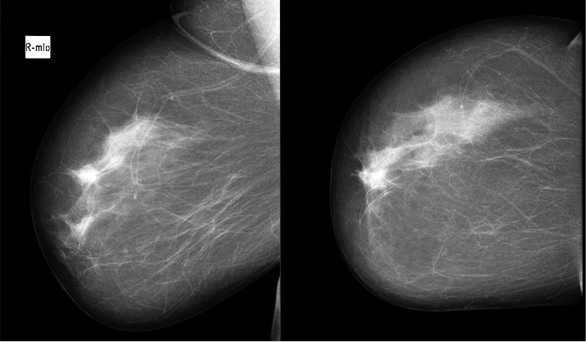
Fig. 2. Local hyperdense zone was seen in mammogram
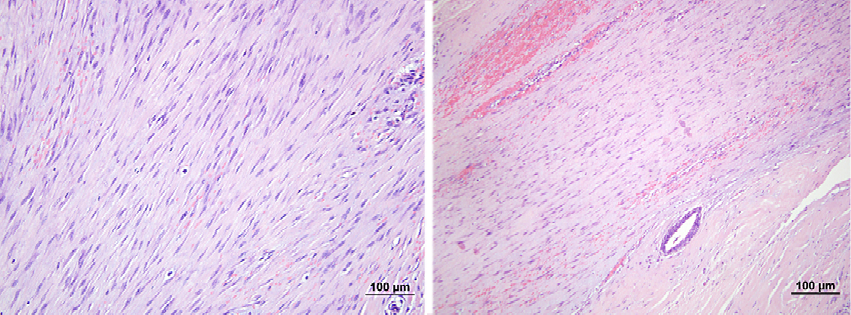
Fig. 3. Microscopic pathological findings revealed spindle cells among collagen depositions (HE staining)
Discussion
Desmoid tumour can occur anywhere in the body. However, their aetiology is still unknown [7]. Physical, hormonal and genetic factors have an important role in desmoid tumours’ development [7].
Desmoid tumour of the breast is extremely rare: it is found in only 0.2% of breast tumours [1]. Most commonly it is found in one breast; however, both breasts may be affected [1]. Desmoid tumour of the breast may be sporadic, but also it may occur after surgical trauma, implantation of silicone breast implants or may be associated with Gardner’s syndrome [2]. Breast fibromatosis may be associated with elevated estrogen levels during pregnancy [2, 9]. In our case, desmoids type fibromatosis affected only one breast. Moreover, the patient did not have any history of genetic factors or breast surgery.
Breast desmoid tumour may occur primarily from the breast tissue or secondary from the pectoralis major muscle [1, 2]. They are locally aggressive, however, do not metastasize [7].
Clinically breast fibromatosis presents as firm, painless mass [4, 8]. Nipple, skin retraction may be seen [2, 4, 8]. On ultrasound images, desmoid tumour typically appears as hypoechogenic, ill-defined mass [1, 8]. In our case, tumour also was firm, not tender, with echoscopically seen ill-defined margins.
Mammographically breast desmoid tumour appears as a speculated mass [4, 8]. Moreover, rarely it may demonstrate calcified deposits [4]. Magnetic resonance imaging (MRI) is the best radiological diagnose method for diagnosing desmoid tumour [5]. On MRI images desmoid tumour may look as ill-defined hypointense or isointese masses on T1-weighted images or hyperintense masses on T2-weighted images [2].
Clinically and radiologically diagnose desmoid tumour of the breast is difficult because it may mimic breast carcinoma [3, 4]. Conclusive diagnose is made just after histopathological examination of the lesion. Macroscopically the lesion appears as greyish-white, firm consistency, irregular, nodular mass [1, 6]. Microscopically spindle cells are seen with varying amount of collagen fibres deposition [2, 7]. Immunohistochemistry is positive for vimentin, actin, but negative for desmin, cytokeratin, S-100, CD 34 [1, 5, 7]. Histopathologically desmoids tumour must be differentiated from the scar formation, fibrosarcoma or fibromatosis – like metaplastic spindle cell tumour [2].
The treatment of breast desmoid tumour is still controversial because of little data due to low incidence of disease [1]. Surgery, radiotherapy, chemotherapy, hormonal therapy may be used for the treatment [1, 4, 5]. Radical surgical excision is the treatment of choice [5, 9]. However, sometimes the complete excision could be avoided in carefully selected patients because the surgery might have poor functional and cosmetic outcomes (i.e. when superficial and subareolar lesion is present, which may require nipple areolar complex removal) [1]. Desmoid tumours have a tendency to recur [6]. They usually recur within 3 years of excision, and then radical excision is required [2]. Wide local resection prevents or reduces the recurrence of disease [8]. When patients have tumour that is unresectable or require extensive surgical resection (i.e. major chest wall resection) radiotherapy might be performed [4]. Systemic therapy may be used in unresectable, recurrent desmoid tumour [7, 9], also for the patients that cannot tolerate surgical treatment and when chest wall is involved [9]. Systemic therapy includes non-cytotoxic (hormonal therapy with Tamoxifen alone or in combination with nonsteroidal anti-inflammatory drugs) and cytotoxic approaches (chemotherapy) [9]. According literature, desmoid tumour may be treated with Tamoxifen due to the fact that fibromatosis may have been related to elevated estrogen levels during pregnancy: treatment with Tamoxifen is associated with reduced size of the tumour [9]. However, postoperative antihormonal therapy does not reduce the local recurrence rate [2]. Methotrexate and/or vinblastine/vinorelbine or an anthracycline-based regimen might be used as “low dose” chemotherapy for desmoids treatment [10]. Targeted therapy (drugs such as imatinib, sorafenib, pazopanib) is a quite new treatment method [10]. Cryoablation also might be used as alternative treatment for local control of small or moderately sized extra-abdominal desmoid tumours [10]. In our case the patient has undergone successful surgery without any adjuvant treatment.
Case report is written according CARE guidelines [11].
Conclusions
Breast desmoid tumour is a rare disease. Clinically and radiologically it may mimic breast carcinoma. Conclusive diagnose of desmoids tumour is made after histopathological examination of the lesion. First treatment of choice is wide surgical resection of the lesion. However, treatment such as radiotherapy, chemotherapy, hormonal therapy may be used.
Our case report presents a rare breast desmoid tumour which was successfully treated with local surgical excision without disease recurrence of two years follow up. We believe that small breast desmoid tumours might be treated with wide local excision with clear margins. In such cases aggressive surgical treatment might be avoided considering that breast desmoid tumour is a benign disease. Moreover, each surgeon must consider the cosmetic result of the surgical procedure. We recommend avoid aggressive surgical treatment while treating small breast desmoid tumours. Mastectomy or other extensive surgical procedure might worsen the quality of patient’s life. However, when extensive chest wall resection is necessary to achieve a complete resection radiotherapy or systemic therapy should be considered.
Acknowledgments
We are grateful and appreciate the assistance of doctor Daiva Cepuliene, Department of Surgery, Medical Academy, Hospital of Lithuanian University of Health Sciences, Kaunas, Lithuania.
References
1. Wongmaneerung P, Somwangprasert A, Watcharachan K, Ditsatham C. Bilateral desmoid tumor of the breast: case seriesand literature review. International Medical Case Reports Journal 2016; 9: 247. https://doi.org/10.2147/imcrj.s106325
2. Erguvan-Dogan B, Dempsey PJ, Ayyar G, Gilcrease MZ. Primary desmoid tumor (extraabdominal fibromatosis) of the breast. American Journal of Roentgenology 2005; 185(2): 488–489. https://doi.org/10.2214/ajr.185.2.01850488
3. Muñoz-Atienza V, del Carmen Manzanares-Campillo M, Sánchez-García S, Pardo-García R, Martín-Fernández J. Fibromatosis breast in the male. Case report. Cir Cir 2013; 81: 211–213.
4. Ha KY, DeLeon P, Hamilton R. Breast fibromatosis mimicking breast carcinoma. Proceedings (Baylor University. Medical Center) 2013; 26(1): 22. https://doi.org/10.1080/08998280.2013.11928903
5. Seo YN, Park YM, Yoon HK, Lee SJ, Choo HJ, Ryu JH. Breast fibromatosis associated with breast implants. Japanese journal of radiology 2015; 33(9): 591–597. https://doi.org/10.1007/s11604-015-0461-y
6. Privette A, Fenton SJ, Mone MC, Kennedy AM, Nelson EW. Desmoid tumor: a case of mistaken identity. The breast journal 2005; 11(1): 60–64. https://doi.org/10.1111/j.1075-122x.2005.21679.x
7. Joglekar SB, Rose PS, Sim F, Okuno S, Petersen I. Current perspectives on desmoid tumors: the Mayo Clinic approach. Cancers 2011; 3(3): 3143–3155. https://doi.org/10.3390/cancers3033143
8. He P, Cui LG, Lei YT, Liu JY, Wang JR. Ultrasound Elastographic Findings of Mammary Fibromatosis. Case reports in radiology, 2015. https://doi.org/10.1155/2015/829468
9. Plaza MJ, Yepes M. Breast fibromatosis response to tamoxifen: dynamic MRI findings and review of the current treatment options. Journal of radiology case reports 2012; 6(3): 16. https://doi.org/10.3941/jrcr.v6i3.897
10. Kasper B, Baumgarten C, Bonvalot S, Haas R, Haller F, Hohenberger P, Moreau G, van der Graaf WT, Gronchi A; Desmoid Working Group. Management of sporadic desmoid-type fibromatosis: a European consensus approach based on patients’ and professionals’ expertise – a sarcoma patients EuroNet and European Organisation for Research and Treatment of Cancer/Soft Tissue and Bone Sarcoma Group initiative. European Journal of Cancer 2015; 51(2): 127–136. https://doi.org/10.1016/j.ejca.2014.11.005
11. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; the CARE Group. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. BMJ Case Rep. 2013. https://doi.org/10.1037/t29881-000