Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2019, vol. 18(4), pp. 254–258 DOI: https://doi.org/10.15388/LietChirur.2019.18.18
Hydatid Cyst Migration in Peritoneal Cavity: A Case Report
Petar Markov
Goce Delcev University, Stip, Macedonia
E-mail: petar.markov@ymail.com
Ilija Milev
Department of General Surgery, Clinical Hospital, Stip, Macedonia
E-mail: ilijamilev@yahoo.com
Aleksandar Mitevski
Goce Delcev University, Stip, Macedonia
Department of Digestive Surgery at General Hospital RE-MEDIKA, Skopje, Macedonia
E-mail: aleksandar.mitevski@ugd.edu.mk
Abstract. Introduction. Cystic echinococcosis is a zoonosis caused by the larval stage of Echinococcus granulosus. In most of cases hydatid cysts are found in the liver but in rare cases a migration of the hydatid cyst can occur following rupture of hepatal pericist.
Case. A 38 year old female presented with abdominal pain, fatigue, weakness and fever for more than three months. Computed tomography show segment II and IV hepatic per-magna cystic formations with dimensions: No I: 80×60×74 mm and No. II: 70×60×58 mm. Per magna cystic formation in the Douglas space, with dimensions of 93×90×62 mm with clearly expressed mass effect on surrounding organ structures.
Discussion. Active hydatid disease may show migration of cysts due to rupture of hepatal pericyst, pressure difference between the anatomic cavities, and by contribution of gravity. Sudden death, anaphylactic shock and dissemination of disease can be seen with cystic content spillage into the peritoneal cavity.
Conclusion. Migrated hydatid cysts are very rare parasitic manifestation presenting with symptoms deriving from the neighboring organs. They are diagnosed typically by CT and managed with evacuation of cysts following abdominal exploration. Full abdominal organ ultrasonography, with accent on the liver, should be performed in any case of intraabdominal simple cyst presence.
Key words: hydatid, cyst, rupture, migration.
Received: 2019 /07/15, Accepted: 2019/09/01.
Copyright © 2019 Petar Markov, Ilija Milev, Aleksandar Mitevski. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Cystic echinococcosis (hydatid disease) is a zoonosis caused by the larval stage of Echinococcus granulosus. Infection with echinococcal organisms is the most common cause of liver cysts in the world [1]. In humans 50–75% of the cysts occur in the liver, 25% are located in the lungs and 5–10% distribute along the arterial system [2]. In rare cases a migration of the hydatid cyst can occur following rupture of hepatal pericist. The hydatid cyst than most frequently migrates to the lower parties of the abdominal cavity mimicking a cyst of the organ that superposes [1, 3].
Case
A 38 year old female presented with abdominal pain, fatigue, weakness and fever for more than three months was admitted to our hospital. During that period she was investigated in favor of complicated urinary infection which was treated conservatively. She has a history of two successful pregnancies and one artificial abortion. Denies food or medication allergies.
The physical examination showed tenderness in the right subcostal region and tenderness in deep palpation of infraumbillical region. The laboratory findings had shown no significant deviations except the value of the CRP (127.4 mg/L).
A transvaginal ultrasonography examination was performed of which a cystic structure is observed in Douglas space. Also an abdominal ultrasonography was made confirming the presence of two oval cystic formations in the liver.
Ca 125, Ca 19-9, Ca 72-4 tumor markers were ordered that were in the normal range values (Ca 125-16.4 U/ml, Ca 19-9-3.01 U/mL, Ca 72-4-1.0).
An CT scan of the abdomen was performed and were found two cystic liver formations, also a cystic formation was verified in the pelvis. The native series of the abdominal CT have shown a segment II and IV hepatic per-magna cystic formations with dimensions: No I: 80×60×74 mm (Figure 1) and No. II: 70×60×58 mm (Figure 2). The changes are with a pericystic reaction of a hypodense character. The formation in the second hepatic segment had a visible mass effect on the stomach. In post contrast series, cystic liver formations were shown as hypodense, hypovascular structures with a clearly expressed contrast accumulation in the cystic membrane and with a demarcation of the pericystic reaction. Per magna cystic formation with hypodense character was also detected at the level of the small pelvis, retrouterine, in the Douglas space, with dimensions of 93×90×62 mm (Figure 3). The cyst has a clearly expressed mass effect on surrounding organ structures. Utter in the AVF pressed to the left. The liver cystic formations were with characteristics of Ehcinococcal cyst but with no serological verification.
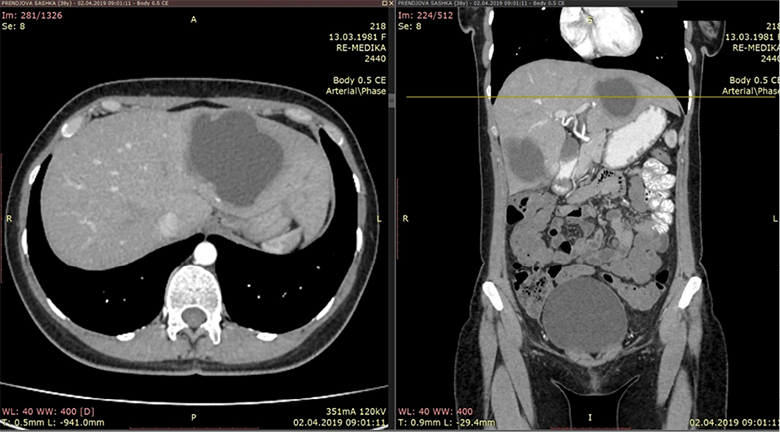
Figure 1. Liver segmet II permagna cystic formation
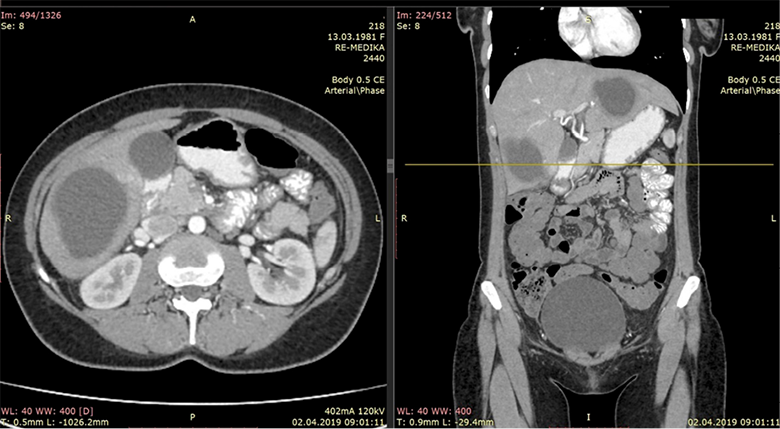
Figure 2. Segment IV hepatic cystic formation
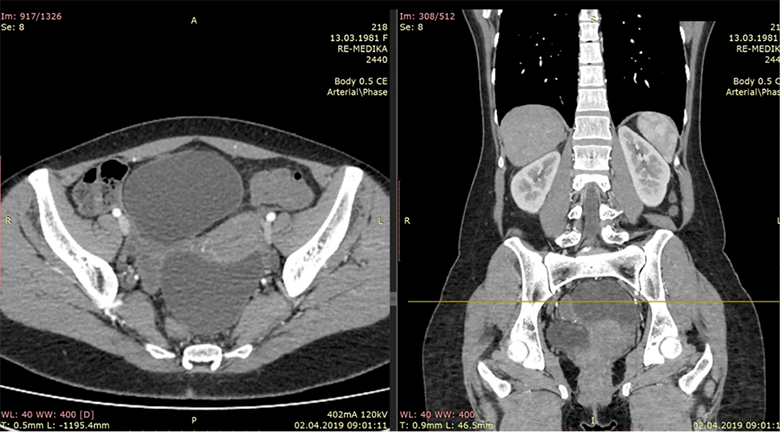
Figure 3. Hypodense cystic formation in small pelvis
The operative planning was in direction of doing median exploratory laparotomy, extirpation of the cystic formation of the lower abdomen and evacuation of the both liver cysts. After performing the required preoperative investigations the patient was operated in general anesthesia.
Median laparotomy was made verifying the echinococcal cysts of the liver. On the visceral side of the fifth segment, an irregular change with adhesions and fibrosis is recorded. It looks alike a periphery of a pericyst above which is the persistant cyst of the V–VI segment. A small adenomatous change of the visceral side of the fifth segment is also noted which is 2 cm in diameter. One cystic formation in germinative membrane only, was found in the small pelvis surrounded with inflamed parts of sigmoid colon, part of the greater omentum and uterus (Figure 4). Evacuation of the cyst was performed. Also, an evacuation of the cysts was performed from the liver. Cysts were opened, the germinative membranes were evacuated and a reduction of pericysts after Papadimitriou was performed. Two omental flaps by the greater omentum were made and inserted in residual cavities of the liver. Two passive drains were applied. An excision of the granulated adenomatous change from the surface of the fifth segment was performed. The drains were extracted on the third and fourth postoperative day.
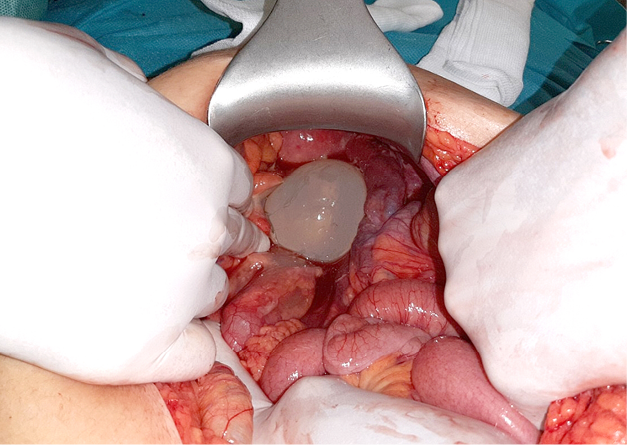
Figure 4. Cystic formation in germinative membrane surrounded with inflamed parts of sigmoid colon,
part of the greater omentum and uterus
Discussion
The liver is the most commonly involved organ with the right lobe being most frequently affected. All types of hydatid cysts can be seen within the liver. They become especially important when they exert a mass effect. The diagnosis is relatively easy in endemic regions and in solitary hydatid cysts. However, a simple liver cysts along with a solitary hydatid cyst in the abdominal cavity can cause diagnostic problems. Living in endemic regions is important clue along with laboratory findings [4].
Active hydatid disease may show migration of cysts due to pressure difference between the anatomic cavities, and in some of the patients, by contribution of gravity. Previous surgery may be a complementary factor for migration. The possibility of migration with hydatid should be considered before surgery [5].
Preoperative diagnosis of hydatid disease is crucial. Sensitivity of serological tests depends on the type of hydatid disease which is positive in 90% of the patients with hepatic hydatidosis while negative in the most of the hydatid diseases in other areas of the body. In atypical cases, ultrasound can diagnose hydatid diseases with 100% sensitivity and specificity [6]. Computed tomography (CT) scan gives a clearer image regarding number, site, size and architecture of the cysts also their relationship with the neighboring structures. In the current case, ultrasound of the abdomen showed features suspicious for hydatidosis or benign neoplasm. Computer tomography imaging confirmed the diagnosis of migrated hydatid cyst.
The rupture of hydatid cysts can be contained (internal), communicating, and direct. Contained or internal rupture occurs when the detachment of the endocyst from the pericyst takes place, but the pericyst remains intact. Internal rupture may be related to degeneration, trauma or response to therapy, and it represents the inactive phase of the hydatid cysts. Communicating rupture implies passage of cystic contents into biliary tracts. When both the pericyst and endocyst rupture, direct rupture occurs. Internal rupture of cyst implies the death of the parasite, but external rupture causes dissemination to other organs. Some hydatid cysts can only rupture externally. Trauma, degeneration and iatrogenic rupture due to surgical and percutaneous treatment cause external rupture. Sudden death, anaphylactic shock and dissemination of disease can be seen with cystic content spillage into the peritoneal cavity [7].
Conclusion
Migrated hydatid cysts are very rare parasitic manifestation presenting with symptoms deriving from the neighboring organs. They are diagnosed typically by CT and managed with evacuation of cysts following abdominal exploration. Full abdominal organ ultrasonography, with accent on the liver, should be performed in any case of intraabdominal simple cyst presence.
References
1. Brunicardi FCh, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Matthews JB, Pollock RE. Schwartz’s Principles of Surgery Tenth Edition, 1285–1286.
2. Jaspal DP. Keyhole Approach for Hepatic Hydatid Cyst Disease in Haryana. International Journal of Contemporary Medical Research 2393-915X; (Print): 2454–7379. ICV: 50.43.
3. Sachar S, Goyal S, Goyal S, Sangwan S. Uncommon Locations and Presentations of Hydatid Cyst. Ann Med Health Sci Res. 2014; 4(3): 447–452.
4. Srinivas MR, Deepashri B, Lakshmeesha MT. Imaging Spectrum of Hydatid Disease: Usual and Unusual Locations. Pol J Radiol. 2016; 81: 190–205.
5. Koc Z, Ezer A. Migrating and herniating hydatid cysts. Eur J Radiol. 2008; 65(1): 120–124. Epub 2007 Apr 23.
6. Salih AM, Kakamad FH, Salih RQ, Rahim HM, Habibullah IJ, Hassan HA, Mikael TM. Hydatid cyst of the thigh: A case report with literature review. Int J Surg Case Rep. 2018; 51: 8–10.
7. Polat P, Atamanalp SS. Hepatic Hydatid Disease: Radiographics Findings. Eurasian J Med. 2009; 41(1): 49–55.