Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2020, vol. 19(3–4), pp. 128–139 DOI: https://doi.org/10.15388/LietChirur.2020.19.32
Comparative Study for Application of Polypropylene Monofilament Light Mesh, Polypropylene Monofilament Heavy Mesh and Self Gripping Polypropylene Mesh in Patients with Inguinal Hernia Surgically Treated with Lichtenstein Technique
Gordana Bozinovks Beaka
Department of Surgery, City General Hospital 8th September, Skopje, Macedonia
E-mail: g.bozinovska_beaka@yahoo.com
Biljana Prgova Veljanovska
Department of Radiology, City General Hospital 8th September, Skopje, Macedonia
E-mail: rasiologija@bolnica.org.mk
Milka Zdravkovska
Faculty of Medicine, Goce Delchev University, Shtip, Macedonia
E-mail: milka.zdravkovska@ugd.edu.mk
Patricija Kalamaras
Department of Infectious Disease, City General Hospital 8th September, Skopje, Macedonia
E-mail: patricijakalamaras@hotmail.com
Abstract. Background / Objective. In our clinical study we have compared the results of intraoperative and postoperative period in patients with inguinal hernia treated operatively with Lichtenstein technique, where one of three different polypropylene meshes has been applied: polypropylene monofilament light mesh, polypropylene monofilament heavy mesh and self gripping polypropylene mesh. Follow up period have been one year. Methods. This study represents randomized, retrospective-prospective, comparative clinical study where 243 patients have been divided into three groups depends of prosthetic mesh that was applied with Lichtenstein technique. We have evaluated the connection between types of used mesh with some of followed parameters: postoperative pain intensity, postoperative patient mobilization, postoperative surgical site occurrences, duration of hospitalization, chronic pain, filling of foreign body in inguinal area and development of recurrences. Results. Patients with applied self gripping polypropylene mesh have significantly lowest pain, lowest hospital stay and lowest duration of surgical procedure than other two groups of patients. In term of chronic pain, only statistically significance we confirmed between the groups of heavy monofilament mesh and self griping polypropylene mesh, where higher number of patients from group with monofilament polypropylene light mesh reported chronic pain. In our study we confirmed that working status and patient age have significant influence on the intensity of postoperative pain in all three patients group. There is no statistical correlation between type of the mesh and surgical site occurrence rate. Conclusion. Patients with applied self gripping polypropylene mesh have significantly lowest pain, lowest hospital stay, lowest duration of surgical procedure and less number of patients experienced feeling of “foreign body” in their groin than other two groups of patients.
Key words: inguinal hernia, Lichtenstein technique, polypropylene meshes, self gripping mesh.
Received: 2020/07/19. Accepted: 2020/09/15.
Copyright © 2020 Gordana Bozinovks Beaka, Biljana Prgova Veljanovska, Milka Zdravkovska, Patricija Kalamaras. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
In western countries 10 to 15% of population have or will have inguinal hernia in some period of life [1].
Inguinal hernia occurs 12 times more often in male than in female [2].
Inguinal hernia repair is one of the most frequently performed operations in general surgery. Tension-free mesh repair currently is the gold standard in inguinal hernia surgery. Tension free techniques are safer, patients have less postoperative pain and discomfort in comparison with tension techniques. Currently, Lichtenstein technique is the most popular technique used by surgeons in inguinal hernia repair [3].
Usage of prosthetic materials decreased the frequency of hernia recurrence, although the chronic pain and feeling of a foreign body in inguinal area after surgery still represent a serious problem which could worsens the level of patient quality of life [4–6].
Main aim of this study is to compare the results of intraoperative and postoperative period in patients with inguinal hernias treated surgically with Lichtenstein technique where used one of three meshes that are compared in this study: polypropylene monofilament light mesh, polypropylene monofilament heavy mesh and self gripping polypropylene mesh.
To evaluate the duration of surgical procedure with the type of used mesh.
To evaluate the connection between types of used mesh with some of followed parameters: postoperative pain intensity, postoperative patient mobilization, postoperative surgical site occurrences, duration of hospitalization, chronic pain, feeling of foreign body in inguinal area and development of recurrences.
Follow up period have been one year.
Material and methods
This study represents randomized, retrospective-prospective, comparative clinical study. In this study, total number of 243 patients were divided in three groups depends of prosthetic mesh that was applied with Lichtenstein technique. N1 group comprises 81 patients where polypropylene monofilament light mesh was applied. N2 group comprises 81 patients where polypropylene monofilament heavy mesh was applied. N3 group comprises 81 patients where self gripping polypropylene mesh was applied.
Inclusion criteria
Age >18 years.
Uncomplicated inguinal hernia without incarceration.
ASA 1–3 classification criteria for anesthesia.
Patient consent for surgical treatment and participation in study.
Body mass index less than 40.
Exclusion criteria
Complicated with incarceration inguinal hernia.
Patient ongoing chemotherapy and immunosuppressive therapy.
Mentally ill patients or patients with cognitive impairment.
ASA 4 classification or higher for anesthesia.
Body mass index greater than 40.
Type of used mesh used in every patient included in the study was randomly done.
Tension free Lichtenstein surgical technique has been performed in every patient included in this study.
Parameters that have been subject of evaluation were: gender, age, body mass index, professional occupation, intraoperative time and postoperative pain.
Postoperative pain was measured indirectly thorough VAS (Visual Analogue Scale). The intensity of postoperative pain was evaluated in different postoperative follow up periods.
Results
From the total 243 patients, 10 were female and 233 were male.
The median age of N1 patients group was 58.81, median age of N2 group was 58.58 and median age of N3 group was 54.93.
Median weight of N1 patients group was 75.09, on N2 group was 77.48 and on N3 group was 77.22.
Median operative time for N1 patients group was 46.05 minutes, for N2 group was 49.32 minutes and for N3 group was 32.41 minutes.
Median postoperative pain measured with VAS was highest in N2 group of patient where polypropylene monofilament heavy mesh was applied (4.78±0.6), lower in N1 group where polypropylene monofilament light mesh was applied (4.48±0.8) and lowest in N3 group where self gripping polypropylene mesh was applied (3.13±0.8).
Median postoperative pain is present in Table 1.
Table 1. Median VAS score in three patient groups
|
|
VAS postoperatively measured |
p value |
|
|
(mean±SD) |
min–max |
||
|
Mesh type |
|||
|
N1 group |
4.48±0.8 |
3–6 |
I вс II вс IIIc p < 0.0001 I вс II sig. I вс III sig. II вс III sig. |
|
N2 group |
4.78±0.6 |
3.5–7 |
|
|
N3 group |
3.13±0.8 |
2–6 |
|
c(Analisys of variance) post-hoc Bonferroni.
Statistically, patients with applied self gripping polypropylene mesh have significantly lower pain than other two groups of patients.
Table 2 represent the median duration of hospitalization for three patients groups.
Table 2. Median duration of hospitalization
|
|
Hospitalization in days |
p value |
|
|
(mean±SD) |
min–max |
||
|
Patient group |
|||
|
N1 group |
4.09±1.3 |
2–8 |
I вс II вс III cp < 0.0001 I вс III sig. II вс III sig. |
|
N2 group |
3.95±1.1 |
2–7 |
|
|
N3 group |
2.78±1.2 |
1–7 |
|
c(Analisys of variance) post-hoc Bonferroni.
Patients with applied self gripping polypropylene mesh have lowest hospital stay with median 2.78 days, in comparison with patient group with monofilament heavy mesh applied 4.09 days and patient group with polypropylene monofilament light mesh with 3.95 days of hospital stay.
Statistically as significant we confirmed the duration of each surgical procedure between the three statistical groups (p < 0.0001).
Post hoc analysis shown that duration of surgical procedure where self gripping polypropylene mesh was applied have been significantly lower then application of two other polypropylene meshes (Table 3).
Table 3. Duration of surgical procedure in minutes
|
|
Duration of procedure in min |
p value |
|
|
(mean±SD) |
min–max |
||
|
|
|||
|
N1 group |
46.05±6.9 |
35–60 |
I вс II вс IIIc p < 0,0001 I вс II sig. I вс III sig. II вс III sig. |
|
N2 group |
49.32±6.0 |
40–60 |
|
|
N3 group |
32.41±5.9 |
20–45 |
|
c(Analisys of variance) post-hoc Bonferroni.
Anamnesis for chronic pain report 16.05% of patients in group with polypropylene monofilament light mesh, 11.11% with implantation of polypropylene monofilament heavy mesh and lowest anamnesis for chronic pain report patients with implantation of self griping polypropylene mesh only 3.7%.
Statistically, these differences as significant were confirmed only between the groups of light monofilament mesh and self griping polypropylene mesh (p = 0.008).
In Table 4 and in Figure 1 we present the duration of chronic postoperative pain in three groups of patients.
Table 4. Distribution of chronic pain in three patients group
|
|
Type of mesh |
p value |
||
|
N1 group |
N2 group |
N3 group |
||
|
Chronic pain (months) (n (%)) |
||||
|
Without pain (n = 218) |
68 (83.95) |
72 (88.89) |
78 (96.3) |
bI вс II p = 0.36 bI вс III p = 0.008** bII вс III p = 0.07 |
|
With pain (n = 25) |
13 (16.05) |
9 (11.11) |
3 (3.7) |
|
|
1 month (n = 12) |
7 |
4 |
1 |
|
|
2 months (n = 8) |
6 |
2 |
0 |
|
|
3 months (n = 3) |
0 |
2 |
1 |
|
|
4 Months (n = 2) |
0 |
1 |
1 |
|
b(Chi-square test); **p < 0.01.
Feeling of “foreign body” had 41.51% of patients in group with monofilament light polypropylene mesh, 39.62% in group with monofilament heavy mesh and 18.88% in patient with self griping mesh.
Perception for foreign body was statistically non significant between two groups with polypropylene monofilament meshes (p = 0.86) but significantly different in comparison between polypropylene self gripping mesh and two groups with polypropylene monofilament meshes (p = 0.018, p = 0.028).
Analysis of duration of feeling of “foreign body” in months, has shown that in group of patient with self gripping polypropylene mesh has no patient that have this feeling more than two months, but in other two groups of patient have one and two patients who had this feeling 9 months after surgical procedure (Table 5).
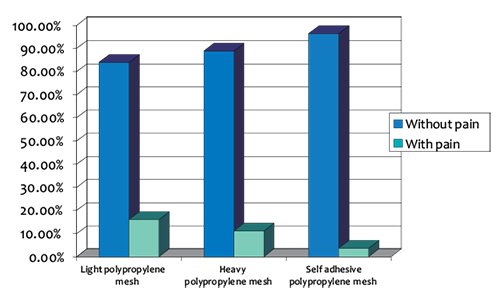
Figure 1. Distribution of chronic pain in three patients group
Table 5. Distribution of patient with foreign body feeling in three patient groups
|
|
Type of mesh |
p value |
||
|
N1 group |
N2 group |
N3 group |
||
|
Foreign body feeling (months) (n (%)) |
||||
|
Without (n = 190) |
59 (72.84) |
60 (74.07) |
71 (87.65) |
bI вс II p = 0.86 bI вс III p = 0.018* bII вс III p = 0.028* |
|
With (n = 53) |
22 (27.16) |
21 (25.93) |
10 (12.35) |
|
|
1 month (n = 26) |
8 |
11 |
7 |
|
|
2 months (n = 19) |
11 |
5 |
3 |
|
|
3 months (n = 3) |
2 |
1 |
0 |
|
|
4 months (n = 1) |
0 |
1 |
0 |
|
|
5 months (n = 1) |
0 |
1 (100) |
0 |
|
|
6 months (n = 3) |
1 (33.33) |
2 (66.67) |
0 |
|
b(Chi-square test); *p < 0.05; **p < 0.01.
Recurrence of inguinal hernia, 12 months after surgery during our follow up period had 3 patients. Two patients from group with monofilament light polypropylene mesh and one patient from group with monofilament heavy polypropylene mesh (Table 6).
In this part from our study we present our results from analysis of influence of demographic characteristics (gender, age, body mass, employment status) of the intensity of postoperative pain in three groups of patient.
In all three groups we do not find out statistically significance in association of gender and intensity of postoperative pain.
All four female patients from the group of monofilament light polypropylene mesh have experienced moderate pain.
In group of monofilament light polypropylene mesh 8 male patient have experienced mild pain (10.39%) and with moderate pain were 69 (89.61%) of male patients.
In the group of monofilament polypropylene mesh, retires and older patient reported higher postoperative pain then unemployed and employees 97.3%, 87.5% and 82.14% respectively.
Table 6. Patient distribution with recurrence of inguinal hernia 12 months after surgery
|
|
Type of mesh |
p value |
||
|
N1 group |
N2 group |
N3 group |
||
|
Recurrence in 12 months follow up period (n (%)) |
||||
|
No |
79 (97.53) |
80 (98.77) |
81 (100) |
aI вс II p = 1.0 aI вс III p = 0.5 aII вс III p = 1.0 |
|
Yes |
2 (2.47) |
1 (1.23) |
0 (0) |
|
a(Fisher exact test).
In the group of monofilament heavy polypropylene mesh all unemployed and employed patients reported mild postoperative pain.
Also, in the same group 96.55% of retires and older patient reported mild postoperative pain.
In the group with polypropylene self gripping mesh unemployed and employed patient reported mild postoperative pain, 88.89% and 66.67% respectively in comparison to retires and older patients who reported moderate postoperative pain 54.17%.
Table 7. Distribution of postoperative pain in three patient group depend from working status
|
Patient group |
Working status |
Intensity of postoperative pain |
||
|
Mild |
Moderate |
Severe |
||
|
I. Monofilament light mesh |
unemployed |
2 (12.5) |
14 (87.5) |
|
|
employed |
5 (17.86) |
23 (82.14) |
|
|
|
retires |
1 (2.7) |
36 (97.3) |
|
|
|
II. Monofilament heavy mesh |
unemployed |
|
12 (100) |
0 |
|
employed |
|
40 (100) |
0 |
|
|
retires |
|
28 (96.55) |
1 (3.45) |
|
|
III. Self adhesive |
unemployed |
8 (88.89) |
1 (11.11) |
|
|
employed |
32 (66.67) |
16 (33.33) |
|
|
|
retires |
11 (45.83) |
13 (54.17) |
|
|
Working status have significant influence on the intensity of postoperative pain in all three patients group (p = 0.0004, p = 0.005, p = 0.014 respectively).
Retires patient from group whit monofilament light polypropylene mesh reported significantly higher postoperative pain score in comparison with unemployed (4.84±0.6 vs 4.25±0.8) and with employed (4.84±0.6 vs 4.14±0.7).
In the group whit monofilament heavy polypropylene mesh retires patient reported significantly higher postoperative pain score in comparison with unemployed (5.05±0.6 vs 4.5±0.5) and with employed (5.05±0.6 vs 4.675±0.4).
In the group with polypropylene self gripping mesh statistical analysis shown that retires patient also reported significantly higher postoperative pain in comparison with unemployed patient (3.44±0.8 vs 2.5±0.7).
In table 8 we present the average score of postoperative pain in three patient groups divided by working status of patients.
Table 8. Average score of postoperative pain in three patient groups divided by working status
|
Patient group |
Working status |
Postoperative pain intensity |
p value |
|
|
mean |
SD |
|||
|
I. Monofilament |
unemployed |
4.25 |
0.8 |
I вс II вс IIIc 0.0004** I вс III sig. II вс III sig. |
|
employed |
4.14 |
0.7 |
||
|
retires |
4.84 |
0.6 |
||
|
II. Monofilament |
unemployed |
4.5 |
0.5 |
I вс II вс IIIc 0.005** I вс III sig. II вс III sig. |
|
employed |
4.7 |
0.4 |
||
|
retires |
5.05 |
0.6 |
||
|
III. Self gripping |
unemployed |
2.5 |
0.7 |
I вс II вс IIIc 0.014* I вс III sig.
|
|
employed |
3.09 |
0.8 |
||
|
retires |
3.44 |
0.8 |
||
c(Analisys of variance) post-hoc Bonferroni.
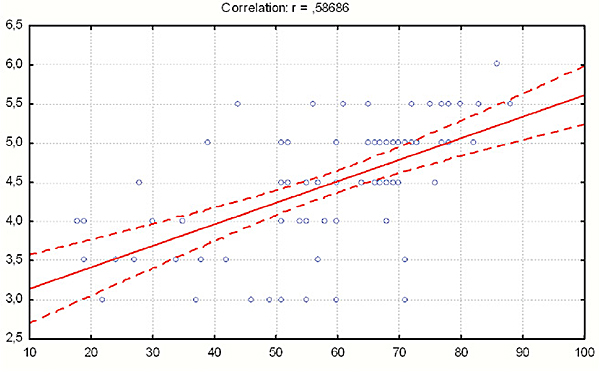
In all three patient groups we have confirmed positive and statistically significant correlation between age of patients and postoperative pain.
With increase of patient ages we notice the increase of postoperative pain.
Thereby the strongest correlation were registered in the group of patient with monofilament polypropylene mesh (r = 0.587) (Table 9).
Table 9. Correlation between postoperative pain intensity and patient’s age in all three patient groups
|
Correlation of postoperative pain vs patient ages |
r |
p value |
|
N1 Group with monofilament light polypropylene mesh |
0.587 |
<0.0001 |
|
N2 Group with monofilament heavy polypropylene mesh |
0.347 |
0.001 |
|
N3 Group with self gripping polypropylene mesh |
0.351 |
0.001 |
Pearson r = 0.587; p < 0.0001; 95% confidence.
Figure 2. Correlation between intensity of postoperative pain and patient’s age in group with monofilament light polypropylene mesh
In this part from our study we present our results from analysis of influence of demographic characteristics (gender, age, body mass, employment status) in appearance of postoperative wound complications in three patient’s groups.
Table 10. Postoperative wound complication divided by gender in three patient’s groups
|
Group |
Gender |
Postoperative wound complication N (%) |
p value |
|||
|
Without |
Seroma |
Hematoma |
Infection |
|||
|
I. Monofilament light polypropylene mesh |
Woman |
4 |
0 |
0 |
0 |
ap = 1.0 |
|
Man |
65 (84.42) |
9 (11.69) |
1 (1.3) |
2 (2.6) |
||
|
II. Monofilament heavy polypropylene mesh |
Woman |
3 (100) |
0 |
0 |
0 |
ap = 1.0 |
|
Man |
64 (82.05) |
9 (11.54) |
4 (5.13) |
1 (1.28) |
||
|
III. Self gripping polypropylene mesh |
Woman |
3 |
0 |
|
0 |
ap = 1.0 |
|
Man |
68 (87.18) |
8 (10.26) |
0 |
2 (2.56) |
||
a(Fisher exact test).
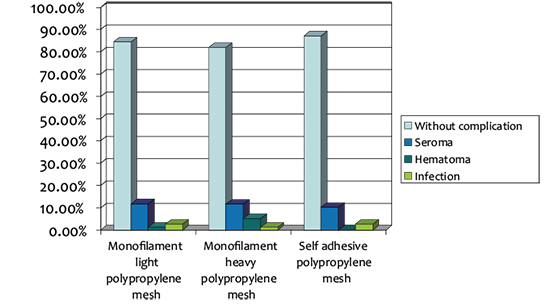
Figure 3. Postoperative wound complication divided by gender in three patient’s groups
Seroma, hematoma and infection of surgical wound as postoperative complication have been registered only in male patients from all three groups of patients. We have shown that there does not have statistically significance between male patients in all three patient groups in presence of early postoperative complications (p = 0.67).
Most frequent complication was occurrence of seroma and this complication has been occurred in 9 male patients in groups with monofilament light and heavy polypropylenes meshes and in 8 patients in group with self gripping polypropylene mesh (Table 10, Figure 3). From 9 patients with seroma in group with monofilament light polypropylene mesh, 1 patient was unemployed, 4 patients were employed and 4 patients were retiree. From 9 patients with seroma in group of monofilament heavy polypropylene mesh, 3 patients were unemployed, 3 patients were employed and 3 patients were retiree. From 8 patients with seroma in group of self gripping polypropylene mesh, 7 patients were employed and 1 patient was retiree.
Hematoma have been observed in one retiree patient from group with monofilament light polypropylene mesh, in 4 patients from group with monofilament heavy polypropylene mesh from which 2 employees patient and 2 retiree patient and none patient with hematoma in group with polypropylene self gripping mesh.
Infection on the surgical wound have been observed in 2 retiree patients from group with monofilament light polypropylene mesh, 1 retiree patient from group with monofilament heavy polypropylene mesh and 2 patient employees from the group with self gripping polypropylene mesh.
Table 11. Postoperative surgical site complication divided by patient ages in all three groups
|
Patient |
Age |
Postoperative wound complication |
p value |
|||
|
Without complication |
Seroma |
Hematoma |
Infection |
|||
|
I. Monofilament |
20–29 |
7 |
0 |
0 |
0 |
ap > 0.05 |
|
30–39 |
5 (83.33) |
1 (16.67) |
0 |
0 |
||
|
40–49 |
4 |
0 |
0 |
0 |
||
|
50–59 |
13 (81.25) |
3 (18.75) |
0 |
0 |
||
|
60–69 |
23 (82.14) |
3 (10.71) |
0 |
2 (7.14) |
||
|
≥70 |
17 (85) |
2 (10) |
1 (5) |
0 |
||
|
II. Monofilament |
20–29 |
4 |
0 |
0 |
0 |
ap > 0.05 |
|
30–39 |
2 |
0 |
0 |
0 |
||
|
40–49 |
7 (70) |
3 (30) |
0 |
0 |
||
|
50–59 |
21 (87.5) |
2 (8.33) |
1 (4.17) |
0 |
||
|
60–69 |
19 (90.48) |
1 (4.76) |
1 (4.76) |
0 |
||
|
≥70 |
14 (70) |
3 (15) |
2 (10) |
1 (5) |
||
|
III. Self gripping |
20–29 |
5 |
0 |
0 |
|
|
|
30–39 |
7 (87.5) |
0 |
0 |
1 (12.5) |
ap > 0.05 |
|
|
40–49 |
13 (86.67) |
2 (13.33) |
0 |
0 |
||
|
50–59 |
12 (70.59) |
4 (23.35) |
0 |
1 (5.88) |
||
|
60–69 |
22 (91.67) |
2 (8.33) |
0 |
0 |
||
|
≥70 |
12 |
0 |
0 |
0 |
||
a(Fisher exact test); b(Chi-square test).
In table 12 we present the results from all three patients group without postoperative complications of the surgical wound divided in median patient ages.
Table 12. Median age of patient with complication of surgical wound
|
Post operative surgical wound |
Age |
p value |
|
|
(mean±SD) |
min–max |
||
|
I. Monofilament light polypropylene mesh |
|||
|
Without complication |
57.94±17.2 |
18–88 |
dp = 0.58 |
|
Seroma |
61.22±11.9 |
39–77 |
|
|
Hematoma |
82.0 |
|
|
|
Infection |
66.05±0.7 |
66–67 |
|
|
II. Monofilament heavy polypropylene mesh |
|||
|
Without complication |
57.75±13.7 |
18–79 |
cp = 0.35 |
|
Seroma |
59.11±13.1 |
41–80 |
|
|
Hematoma |
67.75±7.4 |
58–74 |
|
|
Infection |
73 |
|
|
|
III. Self gripping polypropylene mesh |
|||
|
Without complication |
55.27±15.6 |
20–86 |
dp = 0.9 |
|
Seroma |
54.62±9.2 |
40–67 |
|
|
Infection |
44±12.7 |
35–53 |
|
c(Analysis of variance); d (Student t test).
In this part from our study we present the results from influence of demographic characteristics (gender, age, working status and body mass) in duration of the hospitalization of the patients in all three groups.
Duration of hospital stay has not shown statistical significance in term of patient gender in groups where monofilament light and heavy polypropylene mesh have been implanted.
In the group whit self gripping polypropylene mesh hospital stay have shown statistical significance in term of patients gender (p = 0.033).
Longest postoperative stay have male patient in group with self gripping polypropylene mesh than female patients (2.83±1.2 vs 1.33±0.6) (Table 13).
Table 13. Median duration of hospitalization in all three patient groups
|
Patient group |
Gender |
Duration of hospitalization (days) |
p value |
|
|
(mean±SD) |
min–max |
|||
|
I. Monofilament light |
Female |
3.25±1.9 |
2–6 |
dp = 0.19 |
|
Male |
4.14±1.3 |
2–8 |
||
|
II. Monofilament heavy polypropylene mesh |
Female |
4.33±1.2 |
3–5 |
dp = 0.53 |
|
Maler |
3.93±1.1 |
2–7 |
||
|
III. Self gripping polypropylene mesh |
Female |
1.33±0.6 |
1–2 |
dp = 0.033* |
|
Male |
2.83±1.2 |
1–7 |
||
d(Student test); *p < 0.05.
In this part from our study we present the results from influence of demographic characteristics (gender, age, working status and body mass) in duration of postoperative chronic pain of the patients in all three groups.
Occurrence of chronic postoperative pain we observed only in male patients from all three patients groups.
Most often chronic pain we have observed in the group with monofilament light polypropylene mesh – 13 patients (16.88%), 9 patients (11.54%) from group with monofilament heavy polypropylene mesh and 3 patient (3.85%) from group with self gripping polypropylene mesh
These results we present in Table 14.
Table 14. Chronic postoperative wound pain in all three patient groups divided by gender
|
Patient group |
Gender |
Chronic pain (n (%)) |
p value |
||||
|
Without |
1 month |
2 months |
3 months |
4 months |
|||
|
I. Monofilament light polypropylene mesh |
Female |
4 |
|
|
|
|
ap = 1.0 |
|
Male |
64 |
7 |
6 |
|
|
||
|
II. Monofilament heavy polypropylene mesh |
Female |
3 |
|
|
|
|
ap = 1.0 |
|
Male |
69 |
4 |
2 |
2 |
1 |
||
|
III. Self gripping polypropylene mesh |
Female |
3 |
|
|
|
|
ap = 1.0 |
|
Male |
75 |
1 |
1 |
1 |
|
||
a(Fisher exact test); b(Chi-square test).
Discussion
A tension-free operation with mesh has become the standard technique for inguinal hernia surgery [3]. According to the scientific literature the frequency of hernia recurrence is considerably low after mesh repair [3, 4, 7, 8].
Chronic pain and feeling of a foreign body in inguinal area is the main problems of mesh repair surgery. These complications significantly effect on the quality of patient life [5, 6, 9, 10]. Chronic pain is one of the most serious long-term complications following groin hernia repair [3, 5, 9, 10, 11].
According to out research patients where self gripping polypropylene mesh was applied manifest significantly lower postoperative pain in comparison with other two patient groups.
According to the European Hernia Society guidelines on treatment of inguinal hernia in adult patients, the risk factors for chronic pain are preoperative pain, younger age and severe early postoperative pain [3].
A recent meta-analysis shows that the preservation of the ilioinguinal nerve reduces the incidence of the loss of sensitivity in the inguinal area, but it does not lead to a reduction in chronic pain or in local numbness when compared with their resection [12].
While some authors defend the identification of the different nerves and their preservation, others advocate their resection to reduce the degree of chronic pain associated with these procedures [13].
In patients group where self griping polypropylene mesh has been applied only 3 patients has feeling of “foreign body” two months after surgery.
In group where polypropylene monofilament light mesh has been applied 11 patients have been reported feeling of “foreign body” and 5 patients from the group where monofilament heavy polypropylene mesh reported feeling of “foreign body” in first two months after surgery.
Follow up period shown that patient with applied self gripping polypropylene mesh significantly less have a feeling of “foreign body” in their groin in comparison with other two patient groups.
Another demographic comparative characteristic in our study has shown statistically significant correlation between age of patients and postoperative pain.
With increase of patient ages we notice the increase of postoperative pain.
According to our study, occurrence of surgical site complications in all three groups do not shown statistically difference.
Two parameters, duration of surgical procedure and duration of hospitalization where shorter in group of patient where polypropylene self gripping mesh have been applied in comparison then other two patients groups.
Conclusion
Patients with applied self gripping polypropylene mesh have significantly lowest pain, lowest hospital stay, lowest duration of surgical procedure and less number of patients experienced feeling of “foreign body” in their groin than other two groups of patients.
References
1. Truong S, Pfingsten FP, Dreuw B, Schumpelick V. Value of sonography in diagnosis of uncertain lesions of the abdominal wall and inguinal region. Chirurg 1993; 64(6): 468–475.
2. Bradley M, Morgan D, Pentlow B, Roe A. The groin hernia – an ultrasound diagnosis? Ann R Coll Surg Engl 2003; 85(3): 178–180.
3. Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009; 13(4): 343–403.
4. EU Hernia Trialists Collaboration. Mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 2000; 87(7): 854–859.
5. Kehlet H, Bay-Nielsen M, Danish Hernia Database Collaboration. Nationwide quality improvement of groin hernia repair from the Danish Hernia Database of 87,840 patients from 1998 to 2005. Hernia 2008; 12(1): 1–7.
6. Massaron S, Bona S, Fumagalli U, Valente P, Rosati R. Long-term sequelae after 1,311 primary inguinal hernia repairs. Hernia 2008; 12(1): 57–63.
7. Scott NW, McCormack K, Graham GP, Go PM, Ross S, Grant AM. Open mesh versus non-mesh for groin hernia repair. Cochrane Database Syst Rev 2002; 4: CD002197.
8. van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J. Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J. Surg 2007; 94(4): 506–510.
9. Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, Di Miceli D, Doglietto GB. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 2011; 15(3): 239–249.
10. Paajanen H, Scheinin T, Vironen J. Commentary: Nationwide analysis of complications related to inguinal hernia surgery in Finland: a 5 year register study of 55,000 operations. Am J Surg 2010; 199(6): 746–751.
11. Bringman S, Conze J, Cuccurullo D, Deprest J, Junge K, Klosterhalfen B, Parra-Davila E, Ramshaw B, Schumpelick V. Hernia repair: the search for ideal meshes. Hernia 2010; 14(1): 81–87.
12. Hsu W, Chen CS, Lee HC, Liang HH, Kuo LJ, Wei PL, Tam KW. Preservation versus division of ilioinguinal nerve on open mesh repair of inguinal hernia: A meta-analysis of randomized controlled trials. World J Surg 2012; 36(10): 2311–2319.
13. Alfieri S, Rotondi F, Di Giorgio A, Fumagalli U, Salzano A, Di Miceli D, Ridolfini MP, Sgagari A, Doglietto G, Groin Pain Trial Group. Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg 2006; 243(4): 553–558.