Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2020, vol. 19(3–4), pp. 140–144 DOI: https://doi.org/10.15388/LietChirur.2020.19.33
Adynamic Graciloplasty for Faecal Incontinence in an Adult after Anal Atresia Correction in Infancy – a Case Report
Narimantas Evaldas Samalavicius
Department of Surgery, Klaipeda University Hospital, Klaipeda, Lithuania
Clinic of Internal, Family Medicine and Oncology, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: narimantas.samalavicius@gmail.com
Vitalija Nutautiene
Department of Surgery, Klaipeda University Hospital, Klaipeda, Lithuania
E-mail: vitalija.nutautiene@kul.lt
Lina Butenaite
Department of Rehabilitation, Physical and Sports Medicine, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: lina.butenaite@santa.lt
Rytis Markelis
Department of Surgery, Oncology, Hospital of Lithuanian University of Health Sciences Kauno Klinikos, Kaunas, Lithuania
E-mail: markelis.rytis@gmail.com
Audrius Dulskas
Clinic of Internal, Family Medicine and Oncology, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
Department of General and Abdominal Surgery and Oncology, National Cancer Institute, Vilnius, Lithuania
Faculty of Health Care, University of Applied Sciences, Vilnius, Lithuania
E-mail: audrius.dulskas@gmail.com
Summary. Background. Here we present a case of female patient suffering from bowel incontinence. Case report. The patient underwent unstimulated graciloplasty. Postoperative period was uneventful. After 4 weeks, a course of low frequency electric external stimulation in the area around the neurovascular bundle in the thigh was performed. Patient was evaluated 3 months postoperatively. On inspection, her anus was closed at rest. She stated moderate improvement in her continence and quality of life, her Wexner score was 10 and FISI score was 32 (prior surgery 19 and 44 accordingly). Conclusion. Adynamic graciloplasty seems to be a reasonable method of choice for faecal incontinence.
Key words: unstimulated graciloplasty, faecal incontinence, Wexner score, case report.
Adinaminė graciloplastika išmatų nelaikymui gydyti pacientei po išangės atrezijos chirurginio gydymo vaikystėje: klinikinis atvejis
Santrauka. Įvadas. Straipsnyje aptariamas pacientės, kuri kreipėsi į kliniką dėl išmatų nelaikymo, klinikinis atvejis. Klinikinis atvejis. Pacientei atlikta adinaminė graciloplastika. Pooperacinis periodas buvo sklandus. Praėjus keturioms savaitėms, pacientei taikyta žemų dažnių išorinė elektrinė neurovaskulinio pluošto šlaunyje stimuliacija. Po trijų mėnesių pacientė atvyko į apžiūrą. Apžiūros metu nustatyta užsidariusi išangė. Pacientė teigė, kad išmatų kontrolė pagerėjo (Wexnerio skalė – 10, išmatų nelaikymo rodiklis – 32 (plg. prieš operaciją – atitinkamai 19 ir 44)). Išvada. Adinaminė graciloplastika yra vienas iš patikimų būdų išmatų nelaikymui gydyti.
Reikšminiai žodžiai: adinaminė graciloplastika, išmatų nelaikymas, Wexnerio skalė, klinikinis atvejis.
Received: 2020/05/31. Accepted: 2020/08/01.
Copyright © 2020 Narimantas Evaldas Samalavicius, Vitalija Nutautiene, Lina Butenaite, Rytis Markelis, Audrius Dulskas. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
A large number of perioperative complications, which mostly are infective, technical and functional, as well as modest functional results did not make dynamic graciloplasty a very attractive procedure [1, 2], even bearing in mind that for most of these patients stoma is the only possible alternative. It is related with learning curve effect and complexity of the procedure itself. The reasonable idea seems to be to substitute electrostimulation effect without implantation of sophisticated device simply by applying external electric stimulation postoperatively [3].
Here we present a case of adynamic graciloplasty for faecal incontinence in an adult after anal atresia correction in infancy.
Case report
The study was approved by Institutional review board at Klaipeda University Hospital.
Patients has given written informed consent.
A female patient, born 1969, was referred because of faecal incontinence and mucosal prolapse in September 2017. Patient was born with anal atresia, underwent single attempt of repair during infancy – Romualdi procedure [4] was performed. But whole life she was suffering of faecal incontinence.
Patient was investigated. At rest, anus was opened for 1,5–2 centimetres, and on straining there is a semi-circular prolapse of several centimetres of rectal mucosa of anterior wall. Proctoscopy did not reveal any additional pathology, and colonoscopy was normal. Despite these symptoms were from early childhood and patient lived with them, now patient claimed impaired quality of live and social adaptation restrictions, and was seeking for solution of her condition.
Prior our surgery, her Wexner score was 19 and FISI index was 44.
Patient was operated on November 2017, an unstimulated graciloplasty was performed. The operation was carried out in lithotomy position. Through three short separate incisions in the right thigh gracilis muscle was harvested with the tendon (Fig. 1) up to the level where anterior branch of obturator nerve enters the muscle, in proximity to vascular pedicle – terminal branch of circumflex femoral artery (Fig. 2) approximately 10 cm below pubic tubercle. The muscle was threaded forward to the perineal area were oval incision was made and wrapped around the anus using additional small incision below the tip of the coccyges (Fig. 3), and tendon of the gracilis muscle was fixed with the 1.0 nylon interrupted sutures to the periosteum of lower surface of ischial tuberosity on the same side (right side). Meticulous haemostasis was performed and wounds closed in layers, a Penrose drain left in the bed of the gracilis muscle in lower thigh for 24 hours. Postoperative course was uneventful.

Figure 1. Short separate incisions in the right thigh are performed to harvest gracilis muscle
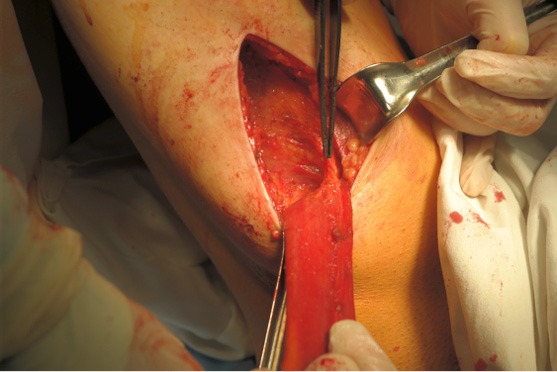
Figure 2. Gracilis muscle is harvested up to the level where anterior branch of obturator nerve enters the muscle, in proximity to vascular pedicle – terminal branch of circumflex femoral artery (approximately 10 cm below pubic tubercle)

Figure 3. The muscle is threaded forward to the perineal area were oval incision is made and wrapped around the anus using additional small incision below the tip of the coccyges
After 4 weeks, a course of low frequency electric external stimulation in the area around the neurovascular bundle in the thigh was performed. We use manometric biofeedback – it measures anal canal pressure (by means of balloons, perfused catheters, or solid-state probes) to detect the contraction and relaxation of the pelvic floor muscles. Pelvic floor biofeedback therapy works by training the brain and pelvic muscles to work together to tighten and relax the pelvic floor muscles. Sensors in the vagina or rectum measure the contraction and relaxation of the muscles and patients get visual cues on a computer monitor so that they can learn to better use these muscles. Assess and record both abdominal and rectal propulsion, none, weak, poor, strong etc. The goal of neuromuscular training using biofeedback techniques is to restore a normal pattern of defecation: to correct the dyssynergia or incoordination of the abdominal, rectal, puborectalis and anal sphincter muscles in order to achieve a normal and complete evacuation, to enhance rectal sensory perception in patients with impaired rectal sensation, to combine the previous two mechanisms (training in the coordination of sphincter contractions with rectal sensation). In EMG training, the patient is asked to squeeze and relax without rectal distention, and home exercises in which the patient is required to repeatedly squeeze the pelvic floor muscles (Kegel exercises) are usually added to the training to further strengthen these muscles. We also used stimulation of the gracilis nerve with skin surface electrodes. The treatment is performed by placing two skin electrodes along the musculus gracilis location after the operation. Electrical stimulation was performed using a TENS (Transcutaneous Electrical Nerve Stimulation) device. Biophysical effects are to control pain and to produce muscle contractions. Treatment is typically for 20–30 minutes at a time and 10 days the duration. We used high frequency TENS: pulse rate 75–100 Hz, pulse width narrow, intensity comfortable to tolerance. Our patient performed physiotherapy five times per week for 2 weeks and continued exercises at home for two months. Her pelvic floor muscle function was assessed and trained with pelvic floor muscle function measurement device “Enraf Nonius” Myomed 632 V.
Patient was evaluated 3 months postoperatively. On inspection, her anus was closed at rest. She stated moderate improvement in her continence and quality of life, her Wexner score was 10 and FISI score was 32.
Discussion
External low frequency nerve stimulation can be combined with biofeedback training sessions. There are records in the literature that type II muscle can be transformed into non-fatigue type I muscle by regular electric nerve stimulation. We used external postoperative nerve stimulation technique described by Niriella and Deen [5], as they have as well demonstrated that with this adynamic graciloplasty technique functional results are equivalent to stimulated graciloplasty. Walega et al. [6] made an analysis of their results with end-stage faecal incontinence, seven patients with dynamic and 13 with adynamic graciloplasty. At 12 months, there was significant and similar improvement in both groups, with better squeeze pressures in adynamic graciloplasty group. In conclusion, with much less cost to achieve same results adynamic graciloplasty seemed to be a reasonable method of choice. In analysis of the literature recently done by Barisic and Krivokapic [7], adynamic graciloplasty was effective in on an average 50% of cases, dynamic – approximately 60%, so hardly there was any difference again. Up to date, favourable reports are published in the literature on success of adynamic graciloplasty, mostly from Asia, though as a rule with small sample size and retrospective in nature [8–10]. In our case, as well demonstrated by Shi et al. [9], we used v type of graciloplasty in order to avoid postoperative defecation problems, and we were able to record successful functional outcome.
Conclusions
Adynamic graciloplasty seems to be a reasonable method of choice for faecal incontinence.
Conflicts of interest – none declared.
Funding – none.
Authors’ contributions – Narimantas Evaldas Samalavicius designed the study and wrote the initial draft of the manuscript. Audrius Dulskas contributed to interpretation of data, and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
1. Belyaev O, Müller C, Uhl W. Neosphincter surgery for fecal incontinence: a critical and unbiased review of the relevant literature. Surgery Today 2006; 36(4): 295–303.
2. Mander BJ, Wexner SD, Williams NS, Bartolo DC, Lubowski DZ, Oresland T, Romano G, Keighley MRB. Preliminary results of a multicenter trial of the electricity stimulated gracilis neoanal sphincter. Br J Surg 1999; 86(12): 1543–1548.
3. Zailani MHM, Azmi MN, Deen KI. Gracilis muscle as neoanal sphincter for faecal incontinence. Med J Malaysia 2010; 65(1): 66–67.
4. Romualdi P. Eine Neue Operationstechnick für die Behandlung einiger Rectum-Missbildungen. Langenbecks Arch Dtsch Z Chir 1960; 279: 371–376.
5. Niriella DA, Deen KI. Neosphincters in the management of faecal incontinence. Br J Surg 2000; 87(12): 1617–1628.
6. Walega P, Romaniszyn M, Siarkiewizc B, Zelazny D. Dynamic versus adynamic graciloplasty in treatment of end-stage fecal incontinence: is the implantation of the pacemaker really necessary? 12-month follow-up in a clinical, physiological, and functional study. Gastroenterology Research and Practice 2015; 2015(3): 1–5.
7. Barišić G, Krivokapić Z. Adynamic and dynamic muscle transposition techniques for anal incontinence. Gastroenterology Report 2014; 2(2): 98–105.
8. Kalra GDS, Sharma AK, Shende KS. Gracilis muscle transposition as a workhorse flap for anal oncontinence: Quality of life and functional outcomes in adults. Indian J Plastic Surg 2016; 49(3): 350–356.
9. Chandrakasan C, Reddy V, Reddy D, Musunuru BR, Dasari V, Pagadala NNB. Role of adynamic graciloplasty in intractable fecal incontinence: initial results from tertiary centre in South India. Int Surg J 2016; 3(4): 2146–2149.
10. Shi GG, Wang H, Wang L, Zhang ZX, Wang H. Two different gracilis loops in graciloplasty of congenital fecal incontinence: a comparison of therapeutic effects. Int J Colorectal Dis 2015; 30(10): 1391–1397.