Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2022, vol. 21(1), pp. 29–33 DOI: https://doi.org/10.15388/LietChirur.2022.21.54
A Case Report on the Spontaneous Intraperitoneal Rupture of Urinary Bladder Presenting as Acute Intestinal Obstruction – Lessons Learnt
Vipin Venugopal Nair
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: vipinvenugopalnair@gmail.com
Pawan Sharma
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: drpawansharma55@gmail.com
Swarup Prabhu
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: swarupprb@gmail.com
Simarjit Singh Rehsi
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: simarjitrehsi89@gmail.com
Abstract. Acute intestinal obstruction is a common surgical emergency. Most of the time, the cause lies in the gastrointestinal track. A 19 year old boy presented with clinical features of acute intestinal obstruction and radiological features suggestive of large bowel obstruction was taken up for surgery. During evaluation we found extravasation of urine inside pelvic cavity. Exploratory laparotomy showed intraperitoneal rent in dome of urinary bladder with dense adhesion of omentum kinking the transverse colon causing acute intestinal obstruction. We were surprised to see the resolution of obstruction with excision of omental band. The bladder was repaired and he was relieved of the problem. This article is a rare example of nongastrointestinal cause for intestinal obstruction. Most of these cases are seen by a general surgeon in an emergency setting. Hence this report is to enlighten the medical caregivers about the existence of this rare entity.
Key words: bladder rupture, intestinal obstruction, non-gastrointestinal.
Received: 2022/01/17. Accepted: 2022/03/01.
Copyright © 2022 Vipin Venugopal Nair, Pawan Sharma, Swarup Prabhu, Simarjit Singh Rehsi. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Acute intestinal obstruction is a frequent surgical emergency worldwide. Mainly the aetiology includes mechanical intestinal obstruction due to pathology within the gastrointestinal tract. However, there are many instances where the cause of intestinal obstruction is due to extraintestinal pathology. This case reports intraperitoneal rupture of the urinary bladder leading to mechanical acute intestinal obstruction. The preop diagnosis was confusing, and the presentation was highly suggestive of perforation peritonitis. However, intraoperatively we were taken aback by an element of surprise and taught us that gastrointestinal tract may not be the cause of peritonitis in some cases [1]. We document our difficulties and lessons learnt in managing this case.
Case report
A 19-year-old boy presented to the acute surgical emergency with an alleged history of pain abdomen, distension of the abdomen and obstipation for three days. He was an old case of Grade III traumatic brain injury on percutaneous endoscopic gastrostomy for the last five months. He sustained a closed head injury six months back when he was hit by a truck while walking. He suffered a bilateral small subdural haemorrhage. Falxcine and tentorial subarachnoid haemorrhage were also present. His general condition was suboptimal. There was a history of recurrent urinary tract infections and bladder outlet obstruction. Three months back, he accidentally pulled out the urinary catheter resulting in trauma to the bladder neck and proximal urethra. The injury was managed with a suprapubic cystostomy. Once the urethra healed, an indwelling urinary catheter was placed, for long term use.
On arrival, he was febrile. He was cachexic with a body mass index of 14 kg/M2. On clinical evaluation, he had tachycardia of 150 beats per minute and a temperature of 102-degree Fahrenheit. He was dehydrated along with decreased urinary output. The abdomen was distended with signs of peritonitis (Laboratory investigation summarized in Table 1).
Table 1. Multiple Laboratory variables on Admission and post-operative day five
|
Investigation |
Preop |
Post Op Day 5 |
|
Hemoglobulin (gm/dl) |
14.6 |
12.3 |
|
Total Leucocyte Count (cumm) |
25 100 |
11 500 |
|
Differential Leucocyte count |
||
|
Polymorphs |
92 |
72 |
|
Lymphocytes |
5 |
24 |
|
Monocytes |
1 |
4 |
|
Platelets (lakhs/cumm) |
4.81 |
2.58 |
|
Serum Urea (mg/dl) |
45 |
24 |
|
Serum Creatinine (mg/dl) |
1.32 |
0.60 |
|
Serum Bilirubin (mg/dl) |
0.8 |
0.7 |
|
Serum Sodium (mEq/dl) |
136 |
140 |
|
Serum Potassium (mEq/dl) |
4.2 |
3.3 |
He was resuscitated with 1 500 ml of crystalloids through a left subclavian central line. Contrast-enhanced CT of the abdomen revealed perforation of the urinary bladder and extravasation of free urine into the pelvic cavity. It also revealed pneumointestinalis and grossly dilated bowel loops till mid transverse colon. There was a cut-off point at the level of the mid transverse colon (Figure 1).
Following initial stabilization, he was taken up for emergency exploratory laparotomy. A midline incision was used to enter the abdominal cavity. Intraoperatively, there was gross free fluid inside the abdominal cavity. The consistency was thick and fibrinous. There were multiple intraop purulent fluid collections. There was similar fluid found in the pelvic cavity and also in the right subhepatic space. Bowel loops were grossly oedematous and distended. There were multiple flakes of fibrin deposits over many parts of the bowel loops. The omentum was pulled towards the urinary bladder area with dense adhesions. The pulled omentum was causing a band like constriction on the mid transverse colon and also over the mid part of the small bowel. A single approximately 10×3 mm rent was seen in the intraperitoneal part of the dome of the urinary bladder anterior to the rectum (Figure 2).
A 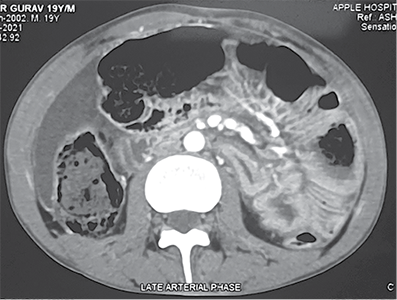 B
B 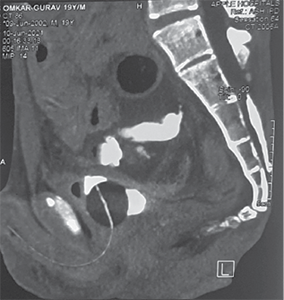
Figure 1. Contrast enhanced computed tomography abdomen pelvis showing A – axial view showing dilated ascending colon, proximal transverse colon, intraperitoneal fluid collection B – extravasation of urine inside peritoneal cavity with pelvic collection
The omentum was pulled towards the urinary bladder area with dense adhesions. The pulled omentum was causing a band like constriction on the mid transverse colon and also over the mid part of the small bowel. A single approximately 10x3 mm rent was seen in the intraperitoneal part of the dome of the urinary bladder anterior to the rectum (Figure 2).
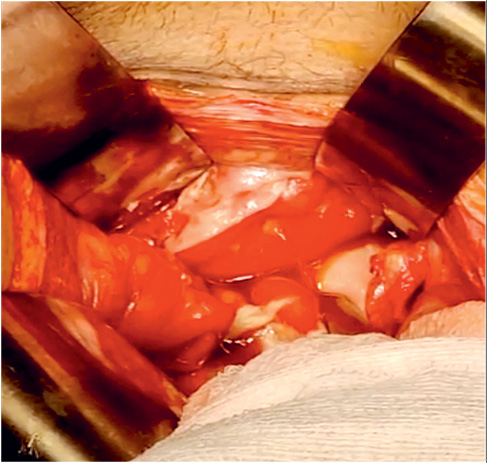
Figure 2. Urinary Bladder with free flow of urine into the peritoneal cavity
Betadine saline was infused into the bladder through an indwelling Foley’s tube to look for any missed perforation. The urinary bladder rent was repaired using 3.0 Vicryl interrupted sutures in two layers. The patency and placement of Foleys were rechecked and there was normal urine output. A thorough search for any other perforation was carried out. The PEG was repositioned and secured with a purse-string suture. Further, it was hitched to the under surface of the anterior abdominal wall with anchoring sutures in a paramedian position.
After a thorough abdominal wash abdomen was closed over pelvic and subhepatic tube drains. Postoperatively he was managed in a high dependency unit with close monitoring, specifically for possible abdominal compartment syndrome. His recovery was uneventful. Anti-seizure prophylaxis and anti-embolic prophylaxis was initiated after surgery. He was given adequate pain relief with epidural analgesia. Inj Tigecycline 50 mg twice daily and Injection Teicoplanin 200 mg twice daily were administered for 5 days.
His recovery was gradual. The subhepatic drain was removed on postoperative day 3. The pelvic drain was kept for two weeks to check for any urinary leak into the peritoneal cavity. Eventually, he was discharged from the hospital on the fifteenth postoperative day after removal of the pelvic drain. He follow up in the surgical outpatient department weekly for four weeks. He was continued on a silicone-coated urinary catheter due to the neurogenic status of the bladder and was referred to urology for further urinary management.
Discussion
The first case of spontaneous intraperitoneal bladder rupture (SIPBR) was documented in the early 1970s [2]. In another report published in 1984, two cases of generalised peritonitis with intraperitoneal air in long-standing cases of indwelling urinary catheters were described. A similar case was also reported in 2015 as a rare urinary emergency. The main emphasis was the fact that these patients will invariably present to a general surgeon rather than a urologist and hence a high index of suspicion is always warranted in the emergency room by the surgeon on call to suspect and diagnose this rare emergency [3, 4].
The two cardinal mechanisms by which SIPBR occurs is either an increased intra-vesicular pressure or a weakness of the bladder wall. The acute and excessive distension of the bladder results in bladder rupture most of the times. Increased serum creatinine with intraperitoneal free fluid is an indirect indicator for bladder rupture. In all cases, the mainline of management is primarily the identification of the defect. We can inflate the bladder using the indwelling catheter and check for physical leaks. Once the leaking site is identified, the repair needs to be done in two layers. Abdominal cavity lavage and alternate pathway for the drainage of urine is always warranted. In elderly patients, a biopsy from the defect to rule out malignancy is also equally important [5, 6].
There are reports in recent literature on the non-operative management of SIPBR. However, it is difficult to predict the extent of peritonitis in such cases. Laparoscopic repair is a very effective and novel way to manage SIPBR in appropriately selected cases and whenever technically feasible [7].
Conclusion
The occurrence of acute abdomen in any patient with an indwelling urinary catheter needs to be evaluated carefully for a possibility of rupture of the urinary bladder. Clinicians should be aware of this potential complication and always need to keep this differential diagnosis in mind while evaluating an acute abdomen patient with an indwelling urinary catheter.
Declarations
Financial Disclosure – Nil. Ethical approval – Patient consent and ethical approval taken from institutional ethical committee. Conflict of Interest – All authors declare no conflict of interest.
References
1. Desai AY, Palande B, Dhabolkar S, Pai VD. Perforative Peritonitis-Gastrointestinal Tract May Not Always Be the Source. Indian J Surg 2017; 79(2): 160–162. DOI: 10.1007/s12262-016-1460-7.
2. Agapitidis N, Papadopoulos N, Papastamatiou L. A Rare Case of Spontaneous Rupture of the Urinary Bladder. South Med J 1976; 69(2): 244–245. DOI: 10.1097/00007611-197602000-00033.
3. Sawalmeh H, Al-Ozaibi L, Hussein A, Al-Badri F. Spontaneous Rupture of the Urinary Bladder (SRUB). A Case Report and Review of Literature. Int J Surg Case Rep 2015; 16: 116–118. DOI: 10.1016/j.ijscr.2015.09.035.
4. Dubey IB, Mohanty D, Jain BK. Diverse Presentation of Spontaneous Rupture of Urinary Bladder: Review of Two Cases and Literature. Am J Emerg Med 2012; 30(5): 832.e1-3. DOI: 10.1016/j.ajem.2011.02.027.
5. Monsellato I, Morello A, Argenio G, Canepa MC, Lenti LM, Priora F. Spontaneous Bladder Rupture Mimicking a Jejuno-ileal Perforation. G Chir 2018; 34(5): 315–318.
6. Albino G, Bilardi F, Gattulli D, Maggi P, Corvasce A, Marucco EC. Spontaneous Rupture of Urinary Bladder: A Case Report and Review. Arch Ital Urol Androl 2012; 84(4): 224–226.
7. Zonca P, Cambal M, Jacobi CA. Laparoscopic Management of Spontaneous Intraperitoneal Perforation of Urinary Bladder. Bratisl Lek Listy 2011; 112(5): 282–286.