Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2021, vol. 20(3–4), pp. 166–170 DOI: https://doi.org/10.15388/LietChirur.2021.20.49
Laparoscopically Treated Giant Gastric Bezoar Complicated with Large Ulcer in Young Patient
Cemal Ulusoy
Department of General Surgery, Prof. Dr. Cemil Taşçıoğlu City Hospital, Istanbul, Turkey
E-mail: drculusoy@gmail.com
Andrej Nikolovski
Department of Visceral Surgery, University Surgery Clinic “Sv. Naum Ohridski”, Skopje, North Macedonia
E-mail: andrejnikolovski@ymail.com
Giray Yavuz
Department of General Surgery, Prof. Dr. Cemil Taşçıoğlu City Hospital, Istanbul, Turkey
E-mail: giray.yavuz@gmail.com
Tuba Saydam
Department of General Surgery, Prof. Dr. Cemil Taşçıoğlu City Hospital, Istanbul, Turkey
E-mail: tuba.saydam@yahoo.com
Ali İlbey Demirel
Department of General Surgery, Prof. Dr. Cemil Taşçıoğlu City Hospital, Istanbul, Turkey
E-mail: ali.ilbey@gmail.com
Abstract. Gastric bezoars are rare but well known intraluminal formations in the gastrointestinal system. Reports for gastric bezoar treatment include dissolution, endoscopic retrieval and surgery (open and laparoscopic). We are presenting a case of 32 years old male patient presented with giant gastric bezoar complicated with large ulcer. The patient was operated laparoscopically with success. Laparoscopic surgery is safe alternative to open surgery for giant gastric bezoars treatment.
Key words: gastric bezoar, gastric ulcer, laparoscopy.
Received: 2021/05/27. Accepted: 2021/09/01.
Copyright © 2021 Cemal Ulusoy, Andrej Nikolovski, Giray Yavuz, Tuba Saydam, Ali İlbey. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Bezoars are rare but well known intraluminal formations in the gastrointestinal system.
Indigestible in their nature, they are made of ingested hair (trychobezoars), fruit (phytobezoars), drug tablets (pharmacobezoars), concentrated infant milk formula (lactobezoars) and foreign bodies-bezoars [1]. They are predominantly located in the stomach. Due to the chronic contact of the bezoar to the gastric mucosa, pressure occurs resulting in ulcer formation [2]. Reports for gastric bezoar treatment include dissolution, endoscopic retrieval and surgery (open and laparoscopic) [3–5]. We are presenting a case of giant gastric bezoar in young male patient accompanied with large ulcer retrieved laparoscopically.
Case report
A thirty two years old male patient presented to our surgery department with complain of postprandial abdominal pain, early satiety and occasional vomiting episodes. He lost 5–6 kg in the past 6 months. The symptoms were present for the last 1 year. No comorbidity was reported. Previously he underwent a gastroscopy in another hospital where a stomach bezoar and large ulcer was diagnosed (Figure 1). Plain x-ray (Figure 2), computerized tomography (CT) scan (Figures 3 and 4) and gastroscopy were conducted in our institution. The gastroscopic examination reported giant rough bezoar impossible for endoscopic retrieval.
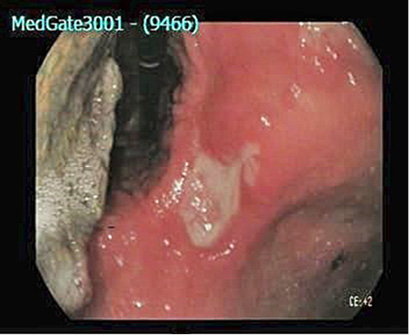
Figure 1. Endoscopic finding of bezoar and large gastric ulcer in the stomach (white arrow)

Figure 2. Plain chest x-ray with visible mass in the stomach
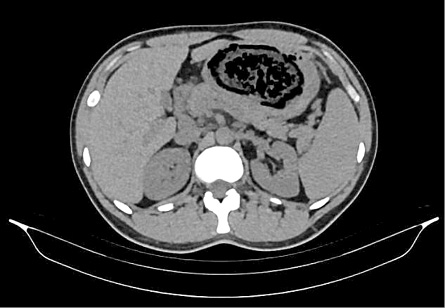
Figure 3. Axial computerized tomography scan with visual bezoar
Laparoscopic removal was offered. Under general anesthesia, a gastroscopy was performed for bezoar visualization. The anterior gastric wall was opened and the laparoscopic view of the bezoar was achieved (Figure 5). It was retrieved from the stomach, inserted in endo-bag and removed from the abdominal cavity through a small transverse laparotomy on the left side of the abdominal wall (Figure 6). Gastrotomy was sutured with laparoscopic linear stapler.

Figure 4. Sagittal computerized tomography scan

Figure 5. Intraoperative finding

Figure 6. Retrieved bezoar
In the first two postoperative days the patient was highly febrile (up to 39 °C). Blood and urine samples were obtained and they were negative for bacterial infection. Serum C-reactive protein value was 247 mg/L. Postoperative CT scan of the thorax and abdomen did not reveal abnormality. Polymerase Chain Reaction (PCR) test was conducted for SARS-Cov-2 infection and it was also negative. The patient was referred to the infectious diseases ward where empiric antibiotic therapy was initiated. On postoperative day 3, inflammation of the surgical wound occurred. It was opened and purulent discharge was freed. The fever subsided the same day. Oral intake of liquid and solid food was conducted. Passage of flatus and stool followed. The patient was discharged on postoperative day 4. The wound was closed according to the principles of delayed wound closure.
Discussion
Although most of the diagnosed bezoars are gastric ones, they are rare clinical entity. The reported prevalence is between 0.068–0.43% [6, 7]. Impaired gastric emptying is believed to be the cause for their formation. Previous gastric surgery, diabetic neuropathy and myotonic dystrophy are the described predisposing factors [8, 9].
Gastric bezoars can be asymptomatic or can present with gastrointestinal symptoms, mostly with abdominal pain, tarry stool, abdominal fullness, nausea, anorexia and hematemesis [2]. The presence of bezoar in the stomach can additionally cause pressure gastric ulcer as a complication [3, 10]. Iwamuro reports a rate of 81.5% of concomitant pressure gastric ulcers in patients with gastric bezoars [2].
Upper endoscopy plays central role in the diagnosis and can also be considered as the method for treatment [4].
Three types of treatment are reported:
• dissolution and irrigation with Coca-Cola, alone or in addition to pro kinetics and lytic enzymes [11];
• endoscopic retrieval with different types of endoscopic devices [12] and surgical removal (open and laparoscopic) [12].
Giant gastric bezoars complicated with pressure ulcers, perforations and gastric obstruction are treated with surgery. Open surgical procedures are reported predominantly [13].
Laparoscopic removal via gastrotomy is another efficient option for this condition [5, 14–17].
One must have in mind that surgery for bezoar that is already complicated caries significant morbidity and mortality. Two small separate series were reported to have a surgical morbidity rate of 28% and 29.4% and mortality rate up to 32.14% and 14.28%, respectively, although, most of the cases in these series were small bowel bezoars [18, 19].
Conclusion
Laparotomy is currently the method of choice for large gastric bezoars removal. Laparoscopy offers safe and effective alternative for this rare entity. Therefore, huge lesions can be removed from the stomach without the need for large laparotomies in order to shorten the postoperative period, reduce postoperative pain and enable better cosmetic results.
References
1. Hall JD, Shami VM. Rapunzel’s syndrome: gastric bezoars and endoscopic management. Gastrointest Endosc Clin N Am 2006; 16(1): 111–119. DOI: 10.1016/j.giec.2006.01.012.
2. Iwamuro M, Tanaka S, Moritou Y, Inaba T, Higashi R, Kusumoto Ch, Yunoki N, Ishikawa S, Okamoto Y, Kawai Y, Kitada K, Takenaka R, Toyokawa T, Okada H. Importance of Second-look Endoscopy on an Empty Stomach for Finding Gastric Bezoars in Patients with Gastric Ulcers. Acta Med Okayama 2017; 71(3): 241–247. DOI: 10.18926/AMO/55207.
3. Khan S, Khan IA, Ullah K, Khan S, Wang X, Zhu LP, Rehman MU, Chen X, Wang BM. Etiological aspects of intragastric bezoars and its associations to the gastric function implications: A case report and a literature review. Medicine (Baltimore) 2018; 97(27): e11320. DOI: 10.1097/MD.0000000000011320.
4. Sultania S, Dhandhu BS, Bhardwaj H, Nijhawan S. Gastric Pharmacobezoar of Mesalamine Tablets Retrieved Endoscopically. ACG Case Reports Journal 2017; 4(1): e31. DOI: 10.14309/crj.2017.31.
5. Ulukent SC, Ozgun YM, Şahbaz NA. A modified technique for the laparoscopic management of large gastric bezoars. Saudi Med J 2016; 37(9): 1022–1024. DOI: 10.15537/smj.2016.9.14590.
6. Mihai C, Mihai B, Drug V, Cijevschi Prelipcean C. Gastric bezoars–diagnostic and therapeutic challenges. J Gastrointestin Liver Dis 2013; 224(1): 111.
7. Kadian RS, Rose JF, Mann NS. Gastric bezoars–spontaneous resolution. Am J Gastroenterol 1978; 70(1): 79–82.
8. LaFountain J. Could your patient’s bowel obstruction be a bezoar? Todays Surg Nurse 1999; 21(2): 34–37.
9. Campos RR, Paricio PP, Albasini JLA. Gastrointestinal bezoars. Presentation of 60 cases. Dig Surg 1990; 7: 39–44. DOI: 10.1159/000171939.
10. Gachabayov M, Abdullaev A, Mityushin P, Gilyazov T. Each worm to his taste: some prefer to eat nettles – a giant gastric phytobezoar. Clin Case Rep 2016; 4(7): 710–711. DOI: 10.1002/ccr3.593.
11. Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther 2013; 37(2): 169–173. DOI: 10.1111/apt.12141.
12. Ugenti I, Travaglio E, Lagouvardou E, Caputi Iambrenghi O, Martines G. Successful endoscopic treatment of gastric phytobezoar: A case report. Int J Surg Case Rep 2017; 37: 45–47. DOI: 10.1016/j.ijscr.2017.06.015.
13. Paschos KA, Chatzigeorgiadis A. Pathophysiological and clinical aspects of the diagnosis and treatment of bezoars. Ann Gastroenterol 2019; 32(3): 224–232. DOI: 10.20524/aog.2019.0370.14.
14. Sharma D, Srivastava M, Babu R, Anand R, Rohtagi A, Thomas S. Laparoscopic treatment of gastric bezoar. JSLS 2010; 14(2): 263–267.
15. Song KY, Choi BJ, Kim SN, Park CH. Laparoscopic Removal of Gastric Bezoar. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2007; 17(1): 42–44. DOI: 10.1097/01.sle.0000213765.86170.77.
16. Shami SB, Jararaa AAM, Hamade AM, Ammori BJ. Laparoscopic Removal of a Huge Gastric Trichobezoar in a Patient With Trichotillomania. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2007; 17(3): 197–200. DOI: 10.1097/SLE.0b013e318058a101.
17. Meyer-Rochow GY, Grunewald B. Laparoscopic Removal of a Gastric Trichobezoar in a Pregnant Woman. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2007; 17(2): 129–132. DOI: 10.1097/SLE.0b013e31802f9ffa.
18. Koulas SG, Zikos N, Charalampous C, Christodoulou K, Sakkas L, Katsamakis N. Management of gastrointestinal bezoars: an analysis of 23 cases. Int Surg 2008; 93(2): 95–98.
19. Erzurumlu K, Malazgirt Z, Bektas A, Dervisoglu A, Polat C, Senyurek G, Yetim I, Ozkan K. Gastrointestinal bezoars: a retrospective analysis of 34 cases. World J Gastroenterol 2005; 11(12): 1813–1817. DOI: 10.3748/wjg.v11.i12.1813.