Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2021, vol. 20(3–4), pp. 177–180 DOI: https://doi.org/10.15388/LietChirur.2021.20.51
A Rare Case Report of Idiopathic Abdominal Cocoon Presenting as Acute Intestinal Obstruction-Management Challenges
Pawan Sharma
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: drpawansharma55@gmail.com
Vipin V. Nair
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: vipinvenugopalnair@gmail.com
Simarjit Singh Rehsi
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: samarjit2005@yahoo.com
Vivek Kumar Singh
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: vivek.singh@gmail.com
Abstract. The idiopathic variant of sclerosing Intraperitoneal fibrosis is a rare pathological entity causing intestinal obstruction. Even though it is described since the beginning of the last century, we are still clueless about the aetiology of this problem. The presentation is often confusing and the clinical and laboratory values will be not confirmatory to establish a diagnosis. A Contrast-enhanced CT scan is a vital investigation of choice. Here we discuss a case of intestinal obstruction with a preop diagnosis of internal herniation, which turned out to be a case of massive intraperitoneal fibrosis. The histopathology was not significant, and no secondary cause was identified. The case report throws wisdom into the existence of this entity and how with a CT scan we can suspect it before surgery. With adequate and meticulous enterolysis we can surgically rehabilitate these patients so that they can lead a normal life.
Key words: idiopathic abdominal cocoon, CT scan, laparotomy, intestinal obstruction, nontubercular.
Received: 2021/07/15. Accepted: 2021/08/26.
Copyright © 2021 Pawan Sharma, Vipin V. Nair, Simarjit Singh Rehsi, Vivek Kumar Singh. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Idiopathic Abdominal cocoon (IAC) is an intraoperative pathology that is very rare in clinical practice. This entity was first observed by Owtschinnikow in 1907 and vividly described by Foo et al. in 1978 [1]. It is also called idiopathic intraperitoneal fibrosis, Sclerosing encapsulating peritonitis and peritonitis chronica fibrosa incapsulata. In tropical nations, it is often seen in young and adolescent girls. The exact aetiology is still not well understood. Here we present a case of IAC which confused the treating team both in diagnosis and management.
Case report
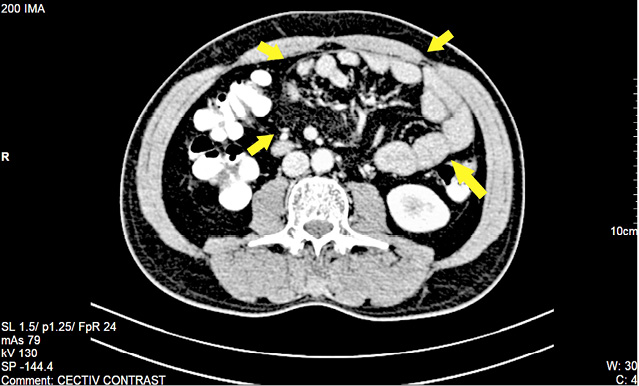
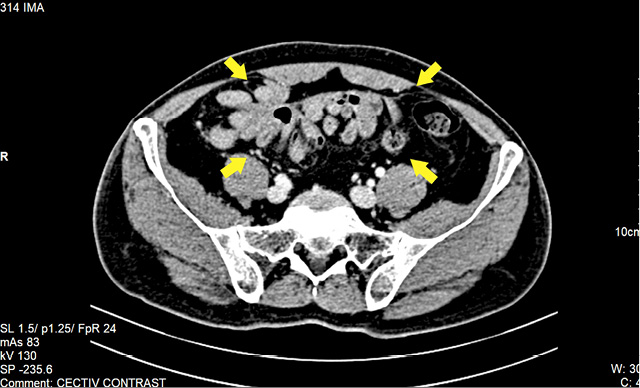
We present a case of a 62-year-old man who presented to the surgical emergency department with complaints of distension of the abdomen and inability to pass stool or gas for 48 hours. He also had three episodes of bilious vomiting. On clinical examination, there was tachycardia and signs of dehydration. The abdomen was distended with absent bowel sounds. He was admitted and started on parenteral intravenous fluid resuscitation. All investigations including hematology and biochemistry were normal. Chest radiograph with both domes of the diaphragm was normal. An abdominal radiograph revealed multiple air-fluid levels suggestive of small bowel obstruction. A contrast-enhanced CT scan of the abdomen revealed dilatation of proximal ileal and jejunal loops with abruptly cut off at the level of the proximal-mid ileal loop. There was circumferential thickening of proximal-mid ileal loops. There was twisting of distal jejunal and proximal ileal loops along with a defect in the mesentery at the level of umbilicus likely to be a small bowel trans mesenteric internal hernia (Figures 1, 2). Abdominal Tuberculosis workup was done with Polymerase Chain Reaction (PCR) for mycobacterium, manteaux test and Cartridge Based Nucleic Acid Amplification Test (CB-NAAT) Sputum were negative. He was managed conservatively with nasogastric decompression with a nasogastric tube, intravenous fluids, and symptomatic drugs. There was partial relief of obstruction after the second day of admission.
Because of the persistent partial obstruction, he underwent diagnostic laparoscopy on the third day of admission for decompression of internal bowel hernia. On attempting to introduce the camera port there was stiff resistance and difficulty in entering the abdomen. There were multiple intraperitoneal adhesions. Laparoscopy was abandoned and the abdomen was explored with midline laparotomy. The entire small gut till IC junction was covered with a thick fibro collagenous membrane that was gradually opened and dissected. The bowel loops within the membrane were also densely adherent to each other and with the mesentery (Figure 3). All the membranes were dissected, and the loops of the intestines were released. There was no perforation of the bowel loop. There were no interloop or intrabdominal collection (Figure 4). Biopsy was taken from the membranous parts and sent for histopathology. The post-operative histopathology was negative for tuberculosis and revealed chronic nonspecific inflammation. The bacterial and viral culture was sent, and the results did not reveal any growth. CB-NAAT of the excised tissue specimen was also negative for tuberculosis. After complete enterolysis, the entire abdominal cavity is thoroughly searched for occult pathology. Once there was no evidence of any structural or infective pathology, the abdomen was closed with a drain in two layers. The post-operative period was uneventful, and the recovery was gradual. He was managed with parenteral nutrition for five days. Following which he was started on an oral diet in a graduated way. He was discharged after seven days with weekly follow up in surgical OPD. As there was no histopathological evidence of tuberculosis, he was not started on anti-tubercular drugs. A gastrointestinal transit study after three months revealed normal functioning of the gut.


Discussion
IAC is a rare and unusual cause of subacute or acute intestinal obstruction. Non-specific symptoms make the diagnosis more difficult. It is commonly seen in young and adolescent girls in tropical countries. However, IAC in males is a very rare cause of intestinal obstruction in males. There are only a few cases published in the medical literature [2]. Even though the aetiology remains obscure various theories proposed includes retrograde menstruation, cell-mediated immunity, or viral infections [3].
Clinical diagnosis is difficult because of non-specific symptoms. Plain radiographs of the abdomen may reveal nonspecific bowel loop dilatation and air-fluid levels. Ultrasound abdomen may reveal a cauliflower or a trilaminar appearance of the bowel. CT has facilitated accurate preoperative diagnosis, long before the patient presents with full-fledged symptoms of acute intestinal obstruction. CT scan is the imaging of choice and plays a significant role in excluding the secondary causes and helps in patient management. The identification of thickened contrast-enhanced peritoneal membrane with encapsulated bowel loops called “cauliflower sign” is a significant finding. CT also helps in identifying the cause and delineating the complications [4–6].
In one of the largest study covering seven years, the abdominal cocoon was documented in seven patients with intestinal obstruction. There was equal sex distribution with more than half of the patient without any valid underlying disease. They concluded that delayed diagnosis could lead to an unfavorable outcome. Early diagnosis with prompt Adhesiolysis and fibrous excision is the key to successful management [7].
Conclusion
Idiopathic abdominal cocoon is a very rare disease-causing intestinal obstruction. The symptoms are mostly nonspecific and preoperative diagnosis is very difficult. CT Scan can guide to exclude other secondary causes. Preoperative diagnosis can only be made if the surgeon is aware of this lesser-known entity and the expected radiological features on a CT scan. Surgery for tissue diagnosis is essential to rule out secondary causes.
Financial disclosure
Authors declare no source of Funding.
Ethical clearance
Institutional ethical clearance obtained, along with consent from the patient.
Conflict of Interest
The authors declare no conflict of interest.
References
1. Tannoury JN, Abboud BN. Idiopathic sclerosing encapsulating peritonitis: abdominal cocoon. World J Gastroenterol. 2012; 18(17): 1999–2004. DOI: 10.3748/wjg.v18.i17.1999.
2. Jagdale A, Prasla S, Mittal S. Abdominal cocoon – a rare etiology of intestinal obstruction. J Family Med Prim Care 2017; 6(3): 674–676. DOI: 10.4103/2249-4863.222040. PMID: 29417033; PMCID: PMC5787980.
3. Calvo PA, de Diego Suárez M, Isnard Blanchar RM, Ojanguren Sabán I, Castellví Gil A. Abdominal Cocoon Syndrome: A Diagnostic and Therapeutic Challenge. Case Report. Cirugía Española (English Edition) 2015; 93(7): e61–e62.
4. Singhal M, Krishna S, Lal A, Narayanasamy S, Bal A, Yadav TD, Kochhar R, Sinha SK, Khandelwal N, Sheikh AM. Encapsulating Peritoneal Sclerosis: The Abdominal Cocoon. Radiographics 2019; 39(1): 62–77. DOI: 10.1148/rg.2019180108. Epub 2018 Dec 7. PMID: 30526331.
5. Vlijm A, Stoker J, Bipat S, Spijkerboer AM, Phoa SS, Maes R, Struijk DG, Krediet RT. Computed tomographic findings characteristic for encapsulating peritoneal sclerosis: a case-control study. Perit Dial Int 2009; 29(5): 517–522. PMID: 19776044.
6. Ethiraj D, Indiran V. Abdominal Cocoon: “Cauliflower Sign” on Contrast-Enhanced Computed Tomography Scan. GE Port J Gastroenterol 2020; 28(1): 76–77. DOI: 10.1159/000507636. Epub 2020 May 19. PMID: 33564710; PMCID: PMC7841799.
7. Çolak Ş, Bektaş H. Abdominal cocoon syndrome: A rare cause of acute abdomen syndrome. Ulus Travma Acil Cerrahi Derg 2019; 25(6): 575–579. DOI: 10.14744/tjtes.2019.48380. PMID: 31701503.