Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2023, vol. 22(2), pp. 81–87 DOI: https://doi.org/10.15388/LietChirur.2023.22.81
Role of Triple Test in Evaluating Breast Lumps
Sajid Iqbal
Department of Surgery, Maharishi Markandeshwer Institute of Medical Sciences and Research, Mullana (Distt-Ambala), Haryana, India
E-mail: drsajid.iqbal@gmail.com
Saima Tabassum
JK Health Department, India
E-mail: drsaima.sajid786@gmail.com
Zahid Khan
Maharishi Markandeshwer Institute of Medical Sciences and Research, Mullana (Distt-Ambala), Haryana, India
E-mail: zahid.khan@gmai.com
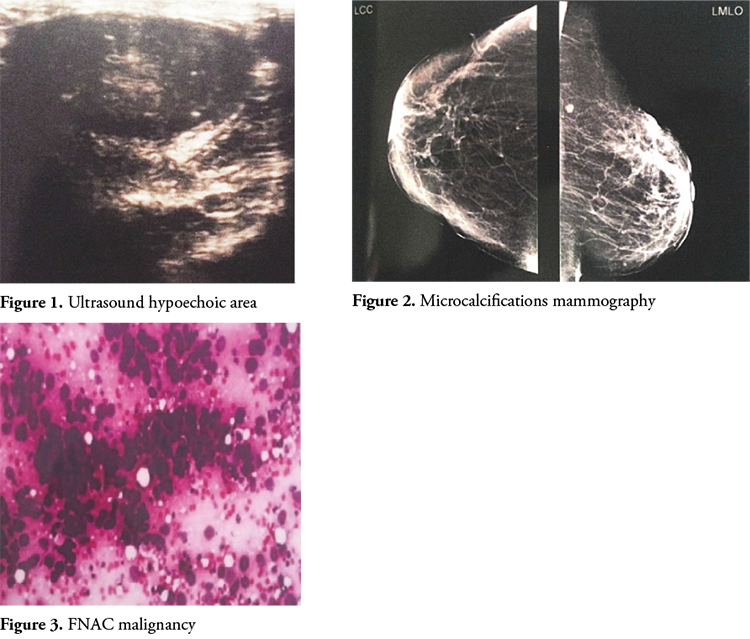
Abstract. Breast tissue undergoes constant physiological changes in a woman’s life because of influence of endocrine hormones during and after reproductive life. These changes may present as pain, lumpiness or both in the breast. Breast lumps are feared for cancer. Thus, it is important for women with a breast lump to receive appropriate evaluation. Clinical breast examination is first step in evaluation of breast lump. The diagnostic sensitivity of clinical breast examination is high (98%) whereas its specificity is low, averaging 48%. Ultrasound is preferred in evaluation of radiologically dense breasts and in the study of breasts with augmentation mammoplasties. Micro-calcifications on mammography are considered to be important signs of breast cancer. X-ray mammography detects microcalcifications in 30–50% of breast cancers. FNAC is a cheap, cost effective and readily available routine diagnostic with a sensitivity ranging between 89% to 98% and specificity between 98% to 100% for palpable breast lumps.
When combined together triple test achieves a higher sensitivity, specificity and diagnostic accuracy than any of the investigations taken alone. We conducted a prospective study to evaluate breast masses by clinical assessment, imaging and pathological examination. Results were compared with histopathology. We concluded that triple assessment in breast lumps gives superior results than any of its modalities taken alone.
Key words: ultrasonography, X-ray mammography, FNAC, triple test, breast self examination.
Received: 2023/01/12. Accepted: 2023/02/26.
Copyright © 2023 Sajid Iqbal, Saima Tabassum, Zahid Khan. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Description of breast lumps started as early as 3000–2500 BC in the Edwin Smith papyrus. Breasts serve an important role in lactation besides giving sexual identity to a woman. Breast diseases are common in females because of more complex structure of female breast, greater volume and influence of endocrine hormones. These changes lead to a number of benign and malignant breast pathologies. Of all breast symptoms, a palpable lump is second most common presentation, pain being the first. Majority of the patients with breast lump suffer from benign breast diseases and cancer accounts for only 10% of cases [1]. The benign breast conditions are not only associated with morbidity but are also of great concern to the patient, in addition to the risk of malignant transformation. Early diagnosis and treatment, besides being life-saving, reduces morbidity [2]. Thus, it is important for women with any breast lump to receive appropriate management. Evaluation and diagnosis of breast lumps involves the clinical history and examination, radiological imaging (ultrasonography and mammography) and pathological assessment (cytological or histological analysis). Together, these parameters, also known as triple test, are highly sensitive in evaluating whether a breast mass is benign or malignant.
Material and Methods
This study was conducted in the postgraduate Department of Surgery, Government Medical College Jammu, from November 2012 to October 2013. Female patients attending the surgical OPD of GMC Jammu and presenting with breast lump(s) were included in study. A detailed patient’s history, focused clinical examination, radiological imaging (mammography, USG) and fine-needle aspiration cytology (FNAC) were used as diagnostic tools. Informed consent was taken for physical examination and investigations giving due respect to maintain the patient’s privacy and keep her comfortable. Subjects not consenting for clinical examination or other radio-pathological investigations, male breast lesions, pregnancy (contraindication to X-ray mammography) and mastitis of pregnancy were excluded from study.
Aims and Objectives
1. To study various breast masses by clinical assessment, imaging and pathological examination.
2. To compare the results with the final surgical diagnosis.
Results
A total of 33 patients took part in this study. Clinical breast examination and breast ultrasound were performed in all the patients. Mammography was done in 25 patients while FNAC was performed on 27 patients. Most patients were in the age group of 30–44. Number of married patients exceeded the unmarried ones (72.7%). Pain with palpable breast lump was second most common presenting symptom, breast lump being the first. Most lumps involved right breast (45.6%), upper quadrant was the most common site involved (57.6%). The relative higher occurrence of breast lump in the upper outer quadrant of breast compared to the other quadrants is because much of the epithelial tissue of breast is present in this quadrant [3].
Clinical breast examination suggested 3 lumps as malignant and 30 as benign. Fibroadenoma was the most common benign mass detected. Aslam also documented fibroadenoma as the most common benign lesion (71.3%) in their study [4].
Sensitivity and specificity of clinical breast examination were found to be 75% and 100% respectively. The negative predictive value of Clinical breast examination was 94.7% while the positive predictive value was 100%. The diagnostic accuracy of Clinical breast examination was 95.45%. The p value of clinical breast examination in our study was less than 0.001 which is statistically significant.
Ultrasonography of the breast suggested 29 cases as benign. Four lumps had features of malignancy on ultrasound. When compared with histopathology for all palpable breast lumps, ultrasound had a sensitivity of 75% and a specificity of 94.12%. The negative predictive value and the positive predictive value were 94.12% and 75% respectively. The diagnostic accuracy of ultrasound for all breast masses was 90.48%. Breast ultrasonography had a concordance value of 90.47%. The p value of USG was 0.005 which is statistically significant.
The sensitivity of mammography for all palpable breast lumps when compared with histopathology in our study was 80% while the specificity was 90.9%. The positive and negative predictive values were 80% and 91% respectively. The diagnostic accuracy of mammography for all breast lumps was 87.5%. The p value of mammography for all breast lumps in our study was 0.006 which is statistically significant. The concordance value of mammography was 87.5%.
FNAC when compared with histopathology for all breast lumps had a sensitivity of 75% and a specificity of 93.3%. The positive predictive value was 75% and a negative predictive value of 93.3% was achieved. The diagnostic accuracy of FNAC in our study was 89.5%. The p value of FNAC was 0.007 which is statistically significant.
When compared with histopathology results, the sensitivity, specificity and the diagnostic accuracy of triple assessment for benign as well as malignant breast lesions in our study model was 100%. (Triple assessment is taken positive if any one of its parameters viz clinical breast examination, radiology and FNAC is positive, while for a negative triple assessment all of its parameters have to be negative.) The results are comparable with most of the previously done studies worldwide.
Discussion
The effective diagnosis and management of breast lesions involves multidisciplinary approach to their assessment. Clinical breast examination may contribute to the earlier detection of breast cancer in women under the age of 40, for whom mammography is not recommended, in women who do not adhere to recommended guidelines for various reasons, and among women who participate in regular screening. However, there is a general observation that smaller tumors have better prognosis than larger tumors [5]. The diagnostic sensitivity of clinical examination is high (around 98%), but the specificity is rather low, averaging 48% [6]. When taken together, clinical breast examination and mammography achieve higher sensitivity than either modality alone for the detection of breast cancer in women of all ages [7]. The clinical breast examination contributes to breast cancer detection independent of mammography [8]. The clinical breast examination can be an important complement to mammography in the earlier detection of breast cancer, presenting as breast lumps. CBE identifies some cancers missed by mammography and provides an important screening tool among women for whom mammography is not recommended or women who do not receive high-quality screening mammography according to recommended guideline [9]. While an accurate and adequate examination, according to the characteristics of the lesion and the patient’s age, increases the cancer detection rate, it also minimizes unnecessary tests and interventions [10].
The presence of micro calcifications can be detected by X-ray mammography in 30–50% of breast cancers [11]. Micro calcifications on mammography are commonly considered to be the important signs of breast cancer, even though they occur in benign conditions as well. X-ray mammography can be false negative in the setting of a palpable breast lump, to the extent of 4% to 12% [12]. Therefore, malignancy cannot be excluded when mammographic findings of a palpable breast mass are negative. A combination of mammography and continuous ultrasound B-scanning of palpable breast masses improves the diagnostic accuracy obtained with mammography alone and aids in the differentiation of non-diagnostic mammograms [13].
Ultrasound is particularly useful in young women with dense breasts in whom mammograms are difficult to interpret, and in distinguishing cysts from solid lesions. It can also be used to localize impalpable areas of breast pathology. Given a known mammographic location, US with a high-frequency transducer can depict breast masses associated with malignant micro calcifications, particularly clusters larger than 10 mm. US can be used to visualize large clusters of micro calcifications that have a very high suspicion of malignancy [14]. Most palpable masses that are not imaged at all by mammography are detectable by ultrasound [15]. BIRADS score helps interpreting the breast lesions sonographically.
Table 1. BIRADS score
|
Birads score |
Diagnosis |
Recommendations |
|
BIRADS 0 |
Diagnosis incomplete, needs further workup (repeat mammography or ultrasonography). |
Further imaging or review of prior studies. |
|
BIRADS 1 |
Negative (N). |
Breasts are normal and routine yearly screening is recommended. |
|
BIRADS 2 |
Benign finding (lymph node, fibroadenoma, implants) – negative (N) mammogram. |
Routine yearly screening recommended. |
|
BIRADS 3 |
Probably benign (>98%) finding (P). |
Repeat mammogram in six months. If there is a family or personal history of breast cancer, additional tests may be advised early. |
|
BIRADS 4 |
Suspicious abnormality (S) probability of malignancy 20% to 35%. |
A biopsy should be considered. |
|
BIRADS 5 |
Highly suspicious of malignancy (M) probability of being cancer >95%. |
Biopsy and treatment. |
|
BIRADS 6 |
Known biopsy – proven malignancy. |
Continue ongoing treatment. |
FNAC of breast lump is an accepted and established method to determine the nature of breast lump with high degree of accuracy [16]. FNAC can reduce the number of open breast biopsies [17]. False-positive diagnosis in aspiration cytology is significantly lower in incidence compared to false-negative cases (0% to 2%). The common lesion giving a false-positive aspirate is ductal hyperplasia or lobular hyperplasia. This finding is also in consonance with the fact that fibrocystic changes and pregnancy-related breast masses account for false-positive findings [18]. FNA should not used as the sole modality and results must be interpreted in correlation with all the clinical and imaging findings (the triple test) to reduce errors and allow proper management for each patient [19].
Table 2. Cytology reporting categories
|
C1 |
Inadequate |
|
C2 |
Benign |
|
C3 |
Atypia probably benign |
|
C4 |
Suspicious of malignancy |
|
C5 |
Malignant |
When compared with histopathology results, the sensitivity, specificity and the diagnostic accuracy of triple assessment for benign as well as malignant breast lesions in our study model was 100%. Similar study was conducted by Masooda Jan and others in Kashmir [20]. They conducted triple assessment on 200 patients with breast lumps without any age restriction. The sensitivity was 100%, specificity 99.3%, positive predictive value 99.3% and negative predictive value was 100%, p value was 0.000 (significant). They had predominantly benign lesions and around 5.5% were malignant. Clinical examination had sensitivity of 99.3%, specificity of 97.8% and p value 0.000. Positive predictive value was 80% and negative predictive value of 99.3%. Mammography done in 137 married females showed sensitivity of 100%, specificity of 97.9%, positive predictive value of 98.1% and negative predictive value of 86.7% USG was done in all 200 patients had almost similar results. FNAC had specificity of 97.1%, 100% sensitivity and 97.3% concordance, positive predictive value of 100% and negative predictive value of 73.3%. They concluded that triple assessment is an effective diagnostic tool to evaluate breast lumps for accurate diagnosis and plan for definitive therapy.
Table 3. The statistical analysis of data
|
|
Histopathology |
p value |
|||
|
Malignant |
Benign |
Total |
|||
|
Clinical |
Malignant |
6 |
0 |
6 |
<0.001 |
|
Benign |
2 |
36 |
38 |
||
|
Total |
8 |
36 |
44 |
||
|
Mammography |
Malignant |
8 |
4 |
12 |
<0.001 |
|
Benign |
0 |
20 |
20 |
||
|
Total |
8 |
24 |
32 |
||
|
FNAC |
Malignant |
6 |
2 |
8 |
<0.001 |
|
Benign |
2 |
28 |
30 |
||
|
Total |
8 |
30 |
38 |
||
|
USG |
Malignant |
6 |
2 |
8 |
<0.001 |
|
Benign |
2 |
34 |
36 |
||
|
Total |
8 |
36 |
44 |
||
|
Triple test (for concordant results) |
Malignant |
4 |
0 |
4 |
<0.001 |
|
Benign |
0 |
14 |
14 |
||
|
Total |
4 |
14 |
18 |
||
Table 4. The statistical analysis of data
|
|
Sensitivity |
Specificity |
PPV |
NPV |
Diagnostic accuracy |
Kappa |
|
Clinical examination |
75 |
100 |
100 |
94.7 |
95.5 |
0.831 |
|
Mammography |
100 |
83.3 |
66.7 |
100 |
87.5 |
0.714 |
|
FNAC |
75 |
93.3 |
75 |
93.3 |
89.5 |
0.683 |
|
USG |
75 |
94.4 |
75 |
94.4 |
90.9 |
0.694 |
|
Triple test (for concordant results) |
100 |
100 |
100 |
100 |
100 |
1.000 |
Conclusion
Accurate history and clinical examination are still the most important methods of detecting breast disease. There are a number of investigations like FNAC and mammography that can assist in the diagnosis and in surveillance of high risk patient. Triple test reliably guides evaluation of palpable breast masses. Benign breast lesions are common than malignant lesions, fibroadenoma and fibrocystic disease are more common in benign disease, whereas intraductal carcinoma accounts for the highest number of malignant lesions. Histological correlation in our study indicated triple test to be better diagnostic tool than FNAC alone. Of all the three components of the triple test, FNAC is the most accurate. A patient with a concordant benign triple test report can be safely followed up without the need for biopsy. The aim of the modified triple test is to allow the clinician to avoid unnecessary open biopsy and to proceed to definitive therapy if a malignant breast lump is present.
It is concluded that triple assessment is valid and a reliable method of diagnosing breast masses. It has a higher sensitivity, specificity and diagnostic accuracy than either of its modalities taken alone. Hence it is recommended that triple assessment should be practiced as the standard diagnostic method to evaluate breast lumps.
References
1. Pattinato G, Panico L, de Rosa NI, Antonio A, Bifano D, Avallone M. Benign lesions of breast. Ann Ital Chir 1997; 62(2): 151–166.
2. Rosa M, Mohammadi A, Masood S. The value of fine needle aspiration biopsy in the diagnosis and prognostic assessment of palpable breast lesions. Diagn Cytopathol 2012; 40(1): 26–34.
3. Tari AK, Monica M. The Breast. In: Greenfield’s Surgery, Scientific Principles and Practice. 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2011, p. 1241–1281.
4. Aslam HM, Saleem S, Shaikh HA, Shahid N, Mughal A, Umah R. Clinico-pathological profile of patients with breast diseases. Diagn Pathol 2013; 8: 77.
5. Michaelson JS, Silverstein M, Wyatt J, Weber G, Moore R, Halpern E, Kopans DB, Hughes K. Predicting the survival of patients with breast carcinoma using tumor size. Cancer 2002; 95(4): 713–723.
6. Crone P, Hertz J, Nilsson T, Junge J, Høier-Madsen K, Kennedy M, Bøjsen-Moller J, Diepeveen P, Hahn-Pedersen A, Jørgensen SJ. The predictive value of three diagnostic procedures in the evaluation of palpable breast tumours. Ann Chir Gynaecol 1984; 73(5): 273–276.
7. Baines CJ, Miller AB. Mammography versus clinical examination of the breasts. J Natl Canc Inst Monogr 1997; 22: 125–129.
8. Barton MB, Harris R, Fletcher SW. The rational clinical examination. Does this patient have breast cancer? The screening clinical breast examination: should it be done? How? JAMA 1999; 282(13): 1270–1280.
9. Oestreicher N, White E, Lehman CD, Mandelson MT, Porter PL, Taplin SH. Predictors of sensitivity of clinical breast examination (CBE). Breast Cancer Res Treat 2002; 76(1): 73–81.
10. Gweon HM, Son EJ, Youk JH, Kim JA, Chung J. Value of the US BIRADS final assessment following mastectomy: BI-RADS 4 and 5 lesions. Acta Radiol 2012; 53(3): 255–260.
11. Black JW, Young B. A radiological and pathological study of the incidence of calcification in diseases of the breast and neoplasms of other tissues. Br J Radiol 1964; 38: 596–598.
12. Kopans DB, Feig SA. False positive rate of screening mammography. N Engl J Med 1998; 339(8): 562–564.
13. Cole-Beuglet C, Beique RA. Continuous ultrasound B-scanning of palpable breast masses. Radiol 1975; 117: 123–128.
14. Moon WK, Im JG, Koh YH, Noh DY, Park IA. US of mammographically detected clustered microcalcifications. Radiology 2000; 217(3): 849–854.
15. Lester SC. The breast. In: Kumar V, Abbas AK, Aster JC, Fausto N, editors. Robins and Cotran Pathologic Basis of Disease. 8th ed. Vol. 23. Philadelphia: Saunders an Imprint of Elsevier, 2010, p. 1068–1069.
16. Purasiri P, Abdalla M, Heys SD, Ah-See AK, McKean ME, Gilbert FJ, Needham G, Deans HE, Eremin O. A novel diagnostic index for use in the breast clinic. J R Coll Surg Edinb 1996; 41(1): 30–34.
17. Hindle WH, Payne PA, Pan EY. The use of fine–needle aspiration in the evaluation of persistent palpable dominant breast masses. Am J Obs Gynaecol 1993; 168: 1814–1818.
18. Ishikawa T, Hamaguchi Y, Tanabe M. False-positive and false-negative cases of fine-needle aspiration cytology for palpable breast lesions. Breast Cancer 2007; 14(4): 388–392.
19. Kaufman Z, Shpitz B, Shapiro M, Rona R, Lew S, Dinbar A. Triple approach in the diagnosis of dominant breast masses: combined physical examination, mammography and fine-needle aspiration. J Surg Oncol 1994; 56(4): 254–257.
20. Jan M, Mattoo JM, Salroo NA, Ahangar S. Triple assessment in the diagnosis of breast cancer in Kashmir. Indian Journal of Surgery 2010; 72(2): 97–103. DOI: 10.1007/s12262-010-0030-7.