Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2023, vol. 22(2), pp. 88–92 DOI: https://doi.org/10.15388/LietChirur.2023.22.82
Internal Hernia Through Foramen of Winslow a Rare Cause of Small Bowel Obstruction: A Case Report
Vipin Venugopal Nair
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: vipinvenugopalnair@gmail.com
ORCID: https://orcid.org/0000-0001-6903-6368
Malik Parmjit
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: paramjeetmalik84@gmail.com
ORCID: https://orcid.org/0000-0002-8265-4491
Pawan Sharma
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: drpawansharma55@gmail.com
ORCID: https://orcid.org/0000-0003-4984-0708
Sarali Santhosh Raja
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: santhoshrajasarali@gmail.com
ORCID: https://orcid.org/0000-0002-0332-0742
Atreya Aprajita
Department of Surgery, AFMC Pune, Maharashtra, India
E-mail: draprajitaatreya@gmail.com
ORCID: https://orcid.org/0000-0002-4181-7522
Abstract. Internal hernia through foramen of Winslow (FoW) is rare condition as there are only 200 cases reported so far in the literature. Our patient a 78 years man presented with a clinical picture suggestive of small bowel obstruction for 5 days. Patient underwent emergency laparotomy following suspicion of internal hernia on imaging. On exploratory laparotomy there was grossly dilated bowel loops and a small segment of terminal ileum and omentum was found herniating through FoW in to the lesser sac. The bowel segment was reduced with gentle traction and herniated segment of omentum was excised due to questionable viability. Opening of FoW was unusually large and to prevent hernia recurrence it was closed partially. Postoperative period was uneventful. This unusual case presented to us diagnostic confusion and management challenge considering the previous history, multiple comorbidities and geriatric profile.
Key words: foramen of Winslow hernia, internal hernias, intestinal obstructions.
Received: 2023/02/03. Accepted: 2023/03/15.
Copyright © 2023 Vipin Venugopal Nair, Malik Parmjit, Pawan Sharma, Sarali Santhosh Raja, Atreya Aprajita. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Majority of bowel obstructions occur in the small intestine (80–90%) and are commonly due to adhesions, abdominal wall hernias, or neoplasm. Internal hernia, defined as the protrusion of abdominal viscera through a peritoneal or mesenteric aperture into a compartment in abdominal or peritoneal cavity is one of the rare cause (<5%) of small bowel obstruction. They are more common after laparoscopic gastric bypass surgeries [1, 2] internal hernia through foramen of Winslow (FoW) is a rare condition. Since the first report in 1834 by Blandin in autopsies, <200 cases have been reported in the medical literature [3].
We report a case of acute intestinal obstruction in an elderly individual due to herniation of small bowel through FoW. The diagnostic and management challenges were highlighted in this article.
Case report
A 78-year-oldmale, a known case of hypothyroidism on irregular thyroxine supplementation, presented with complaints of diffuse pain abdomen, obstipation and progressive abdominal distension for last five days to the surgical emergency room. There was nausea and multiple episodes of bilious vomiting for one day. He also gave a past history of laparotomy twice in 2017 and 2019 for intestinal obstruction.
On arrival to accident and emergency he had tachycardia (pulse – 110 bpm) and was dehydrated. Rest parameters were normal. He was afebrile. Abdominal was grossly distended with generalised guarding on palpation and hyper-tympanic note on percussion. Bowel sounds were absent. Rest of systemic examination was unremarkable
On further evaluation following findings were noted. His lab parameters were: Hemoglobin – 15.3 gm/dl (13–16 gm/dl), Total Leukocyte Count – 6 800/cmm (4 000–11 000/cmm), Platelet Counts – 268 000/cmm (1.5–400 000/cmm), PT/INR – 13.1 sec/1.06 (13–16 sec/1 to 1.3), Urea – 51 mg/dl (15–45 mg/dl), Creatinine – 0.9 mg/dl (0.5–1.3 mg/dl), Na+ – 134 meq/L (135–145 meq/L), K+ – 4.2 meq/L (3.5–4.5 meq/L), 4.5 meq/L, Bilirubin – 1.1 mg/dl (0.1–1.2 mg/dl), AST/ALT – 44 IU/L, 75 IU/L (15–45 IU/L, 15–60 IU/L), Amylase/Lipase – 22 IU/L, 110 IU/L (20–85 IU/L, <300 IU/L), Proteins (Total/Albumin) – 7.2 gm/dl, 4.0 gm/dl (6–8 gm/dl, 3–4.5 gm/dl), T3/T4/TSH – 40 ng/ml, 4.13 ug/dl, 9.39 mIU/L (0.2–2.0 ng/ml, 6–12 ug/dl, 0.3–4.0 mIU/L), HIV – 1&2/HbsAg, HCV – negative.
On X-ray abdomen erect and supine with both domes of diaphragm multiple air fluid levels were seen suggestive of intestinal obstruction. There was no gas under diaphragm (Figure 1A).
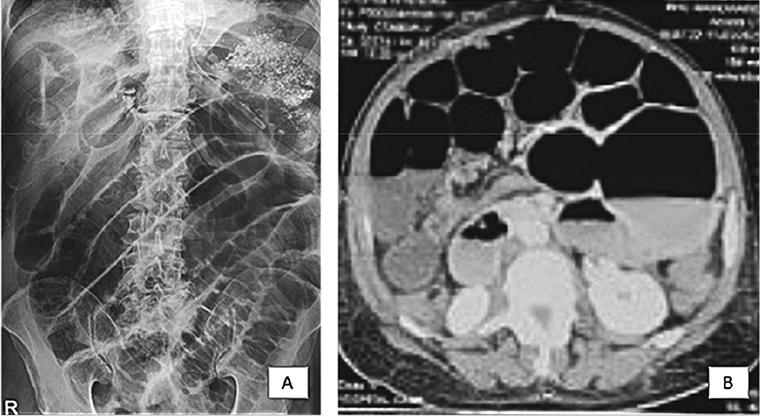
Figure 1. A, B
Underwent CECT abdomen on suspicion of small bowel obstruction. The finding were suggestive of small bowel obstruction with a definitive transition zone at distal ileum and four centimetre dilatation of proximal small bowel loops (Figure 1B).
In view of clinical presentation of intestinal obstruction, he was taken up for emergency exploratory laparotomy under general anaesthesia.
Intraoperative, there was grossly dilated bowel loops of questionable viability. On evisceration of the intestinal loops, there was no faecal or biliary contamination. On further manipulation of the gut, we were able to find a loop of ileum herniating through the lesser sac (Figure 2A). The loops of intestine were so dilated that it prevented the reduction of this internal hernia. We used hot saline mops to reduce bowel oedema. The patient was given 100% oxygen to improve tissue oxygenation. Once the bowels were eviscerated and secured safely an attempt to reduce the hernia was tried. However, the bowel was stuck to the lesser sac. Widening of the sac was done using limited kocherisations. Once the neck of sac was wide enough the herniated loop of intestine was reduced (Figure 2B). The associated necrosed omental segment was excised and tissue send for histopathology (Figure 2C).
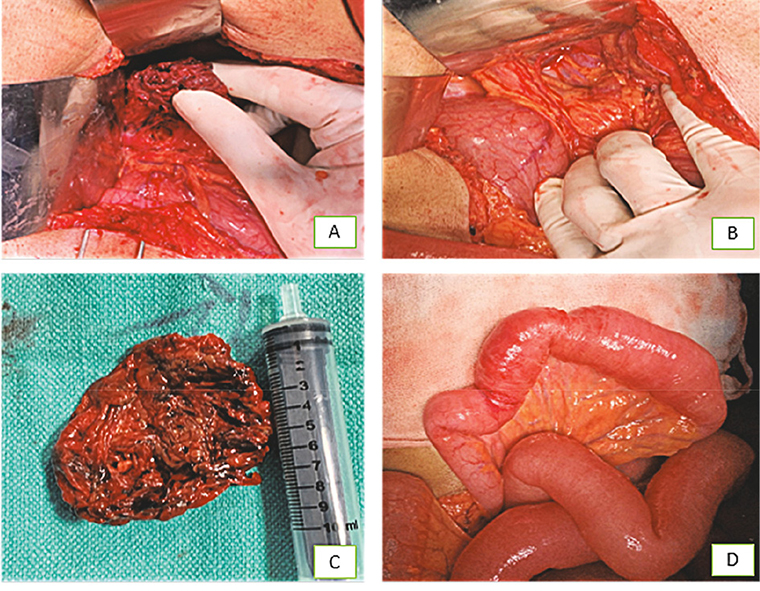
Figure 2. A, B, C, D
After reduction the herniated loop of bowel seemed to be dusky. The bowel was kept in warm saline mops and patient was administered 100% oxygen. There was return of peristalsis and the colour turned pink after 5 minutes (Figure 2D). The decision was taken to close the hernia defect with interrupted Polyglactin (™Vicryl 3.0) sutures. Rest of bowel inspected and no significant abnormality noted. The dilated bowels were preventing abdominal closure. The contents of small intestine were milked retrograde to the stomach and aspirated from the Nasogastric tube through suction. Once the bowel was successfully decompressed the laparotomy wound was closed in layers.
The patient was started on clear oral fluids from second postoperative day and subsequently on soft diet. He was discharged on postoperative day five. Presently patient is doing well on third month of follow-up. The histopathology of the excised omentum revealed normal matured adipocytes with few inflammatory infiltrates. No evidence of giant cell granuloma, atypical or malignant cells seen.
Discussion
There are eight main types of internal hernias, categorized depending on where the hernia occurs. Foramen of Winslow hernia can be defined as peculiar variant of internal abdominal hernia, since it is a normal peritoneal orifice kept closed by normal intra-abdominal pressure that may be permeated by the intra-abdominal viscera. Hernias through the foramen of Winslow are rare and constitute only 8% of internal hernias and 0.08% of total hernias [4, 5].
There are multiple anatomical abnormalities reported as possible predisposing factors for a visceral herniation through this foramen (i) abnormally enlarged foramen; (ii) the presence of an unusually long small-bowel mesentery or persistence of the ascending mesocolon; (iii) an elongated right hepatic lobe, which could be directing the mobile intestinal loop into the foramen; (iv) a lack of fusion between caecum or ascending colon to the parietal peritoneum; (v) a defect in the gastro-hepatic ligament; (vi) incomplete intestinal rotations or malrotation [6].
The rate of preoperative diagnosis has been reported to be <10% of the intraoperatively confirmed cases. A delay in diagnosis and treatment is often observed and may be responsible for the high mortality rate of up to 49% associated with this hernia type. Internal hernia is often revealed by intestinal obstruction associated with non-viable bowel at the time of operation [3]. Symptoms are usually related to bowel obstruction. The severity of the pain is related to the presence of bowel strangulation with subsequent necrosis. In some very particular cases, the internal hernia through the Winslow hiatus is revealed by an obstructive jaundice due to direct compression of the hepatic pedicle [2].
Clinical examination is non-specific and laboratory findings are rarely helpful. The key to diagnosis relies on prompt radiologic studies and the CT scan is nowadays considered the investigation of choice. Various, more or less specific findings have been reported, such as an air-fluid collection in the lesser sac or signs of small bowel obstruction associated with the presence of mesenteric vessels stretching anterior to the inferior vena cava and posterior to the portal vein; the absence of the ascending colon in the right gutter and an antero-lateral displacement of the stomach [7, 8].
The treatment invariably requires urgent surgery, and even if symptoms are limited, it should be considered in order to assess intestinal viability because of the risk of intestinal strangulation. Treatment is based on careful inspection with subsequent hernia reduction that is frequently possible with simple and gentle traction. Occasionally, this can be difficult; in these situation the gastrocolic or gastro-hepatic ligaments must be opened or, alternatively, a wide Kocher manoeuvre performed. In the case of massive colonic dilatation a colotomy for decompression with a suction device can be useful [1, 9]. In the case of overt intestinal necrosis an adequate resection is obviously mandatory; nevertheless there is no clear and established consensus on surgical management when the herniated contents are grossly viable. In our case limited kocherisation for reduction of hernia was performed followed by partial closure of the defect.
Furthermore, in order to prevent recurrent herniation, some surgeons decide to definitively close the foramen of Winslow. This option can however lead to meaningful complications such as accretions and/or portal vein thrombosis. Thus, leaving the foramen open may be justifiable since the inflammatory postoperative adhesions will most often obliterate the foramen entrance with no evidence of recurrent herniation [4].
Conflicts of interest. The author declares no competing interest.
References
1. Sikiminywa-Kambale P, Anaye A, Roulet D, Pezzetta E. Internal hernia through the foramen of Winslow: a diagnosis to consider in moderate epigastric pain. J Surg Case Rep 2014; 2014(6): rju065.
2. Maingot’s abdominal operations. 13th edition. Chapter 38. Small bowel obstruction.
3. Osvaldt AB, Mossmann DF, Bersch VP, Rohde L. Intestinal obstruction caused by a foramen of Winslow hernia. Am J Surg 2008; 196(2): 242–244.
4. González Conde R, Pardo Rojas P, Valeiras Domínguez E, Pérez López C, Santos Lloves R, Gómez Lorenzo FJ. Correct preoperative diagnosis of herniation through the Foramen of Winslow: two case reports. Hernia 2013; 17(3): 409–414.
5. Takeyama N, Gokan T, Ohgiya Y, Satoh S, Hashizume T, Hataya K, Kushiro H, Nakanishi M, Kusano M, Munechika H. CT of internal hernias. Radiographics 2005; 25(4): 997–1015.
6. Moris D, Tsilimigras DI, Yerokun B, Seymour KA, Guerron AD, Fong PA, Spartalis E, Sudan R. Foramen of Winslow Hernia: a Review of the Literature Highlighting the Role of Laparoscopy. J Gastrointest Surg 2019; 23(10): 2093–2099. DOI: 10.1007/s11605-019-04353-3.
7. Huang Y, Qin L, Wu L, Huang Q. An Adolescent with Ileum Herniation Through Foramen of Winslow: A Case Report and Literature Review. Nigerian Journal of Clinical Practice 2022; 25(8): 1372–1376. DOI: 10.4103/njcp.njcp_1778_21.
8. Doishita S, Takeshita T, Uchima Y, Kawasaki M, Shimono T, Yamashita A, Sugimoto M, Ninoi T, Shima H, Miki Y. Internal Hernias in the Era of Multidetector CT: Correlation of Imaging and Surgical Findings. Radiographics 2016; 36(1): 88–106.
9. Akyildiz H, Artis T, Sozuer E, Akcan A, Kucuk C, Sensoy E, Karahan I. Internal hernia: complex diagnostic and therapeutic problem. Int J Surg 2009; 7(4): 334–337.