Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(1), pp. 56–60 DOI: https://doi.org/10.15388/LietChirur.2024.23(1).8
Intrathoracic Displacement of the Humeral Head with Polytrauma: Case Report
Kipras Sasnauskas
Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: kipras.sasnauskas360@gmail.com
Robert Vrublevski
Clinic of Rheumatology, Orthopaedics Traumatology and Reconstructive Surgery, Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: robert.vrublevski@rvul.lt
Povilas Masionis
Clinic of Rheumatology, Orthopaedics Traumatology and Reconstructive Surgery, Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: povilas.masionis@rvul.lt
Sigitas Ryliškis
Clinic of Rheumatology, Orthopaedics Traumatology and Reconstructive Surgery, Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: sigitas.ryliskis@rvul.lt
Abstract. Intrathoracic displacement of the humeral head is rarely documented due to high mortality of the trauma. As a result, there is no clear consensus about how such case should be approached. In this report we reviewed our successful case, and reviewed the literature. The patient arrived after car accident with a broken humerus and upon taking X-ray found to have the humeral head lodged in the chest cavity. After humeral head removal and arthroplasty, patient was discharged without complications. In literature several cases were found in which a patient usually suffers because of high energy trauma with arm typically in abducted position. In all cases treatment involves removing humeral fragment from chest and prosthetic arthroplasty of the glenohumeral joint. Although some authors suggest leaving humeral fragment in some cases while others suggest to always remove. Exact indications of such decision are unclear. Cases like this pose a high risk of neurological and circulatory complications, although no complications were observed in this case. Nevertheless, there have been too few similar cases described to establish a proper methodology.
Keywords: dislocation, humerus, arthroplasty, shoulder.
Intratorakalinis žastikaulio galvos išnirimas, esant politraumai: klinikinio atvejo aprašymas
Santrauka. Intratorakalinis žastikaulio galvos išnirimas – trauma, kuri retai aprašoma dėl didelio mirštamumo, todėl nėra aiškiai sutariama, kaip šią traumą patyrusį pacientą reikėtų gydyti. Straipsnyje aptariamas sėkmingo gydymo atvejis, apžvelgiama mokslinė literatūra. Į gydymo įstaigą dėl lūžusio žastikaulio pristatytas avariją patyręs pacientas. Atlikus rentgeną, nustatyta krūtinės ląstoje įstrigusi žastikaulio galva. Žastikaulio galvą pašalinus iš krūtinės ląstos ir protezavus, pacientas išrašytas gydytis ambulatoriškai, nesant komplikacijų.
Mokslinėje literatūroje aprašyta keletas atvejų, kai pacientai, dažniausiai patyrę didelės jėgos sukeltą traumą, pristatyti į gydymo įstaigą rankai esant abdukcinėje pozicijoje. Visais atvejais trauma gydyta šalinant žastikaulio fragmentą iš krūtinės ląstos ir protezuojant glenohumeralinį sąnarį. Kai kurie tyrėjai siūlo tam tikrais atvejais palikti žastikaulio fragmentą krūtinės ląstoje, kiti rekomenduoja žastikaulio fragmentą visada pašalinti. Minėtų sprendimų aiškių indikacijų nėra.
Straipsnyje pristatomu atveju komplikacijų nenustatyta, tačiau tokios traumos kelia didelį pavojų kraujotakai ir nervinei sistemai. Vis dėlto kol kas aprašytų klinikinių atvejų nepakanka, kad būtų galima nustatyti tinkamą metodologiją šiai traumai gydyti.
Reikšminiai žodžiai: išnirimas, žastikaulis, protezavimas, petys.
Received: 2023/08/28. Accepted: 2023/10/10.
Copyright © 2024 Kipras Sasnauskas, Robert Vrublevski, Povilas Masionis, Sigitas Ryliškis. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Dislocations of the shoulder joint with bone fracture are relatively rare injuries only 20 were documented up to year 2009 [1]. In extremely rare cases, a part or fragment of the bone becomes trapped intrathoracically. These cases are typically caused by high-energy traumas and are accompanied by polytrauma, often involving respiratory, nervous, and circulatory system injuries, making them particularly life-threatening. This article describes one such case following a car accident and reviews similar documented cases and potential complications.
Methods
Analysis of a clinical case (images, examination, treatment) was performed, and a literature review was conducted using the PubMed database. Keywords that were used: shoulder, humeral, dislocation, intrathoracic. Out of 21 publications 10 were reviewed.
Case description
A 58-year-old patient was admitted to the Emergency Department of level I Trauma Center in August 2022 due to polytrauma sustained in a car accident. On arrival, the patient’s condition was severe, with decreased consciousness (GCS score of 12), unstable hemodynamic, subcompensated peripheral circulation, blood pressure of 62/32, and heart rate of 78 beats per minute. There was reduced breathing on the left side with a respiratory rate of 18 breaths per minute and an oxygen saturation (SpO2) of 85.0%. Palpation revealed pain in the left posterior chest. X-rays and CT scans were performed, which revealed a traumatic hemothorax on the left side, humeral head within the pleural cavity, three rib fractures, lung contusion, and hematoma.
Neurovascular status of the left hand was intact. The patient’s condition was stabilized in the intensive care unit and after 5 days transferred to the Thoracic Surgery Department, where 4 days later a resection of the fifth rib, thoracoscopic removal of the humeral head, and lung decortication were performed.
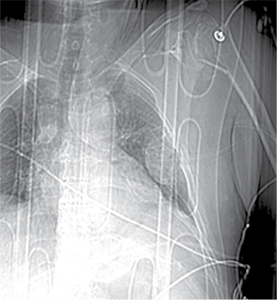
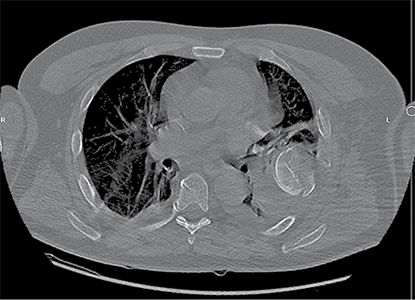
Figure 1. First X-ray and computer tomography upon admission (with humeral head shown)

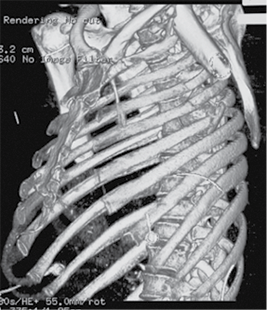
Figure 2. Subsequent 3D reconstruction
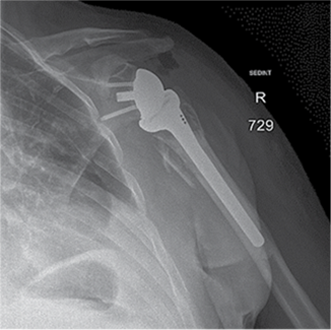
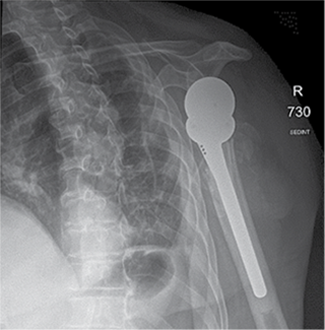
Figure 3. X-ray after shoulder arthroplasty
In a subsequent consultation, it was decided to perform shoulder arthroplasty 11 days later using reverse prosthesis (Delta Xtend, DePuy Synthes) with tuberosity fixation.
Postoperative course was uneventful in the chest or shoulder. The patient was discharged after 23 days from admition.
Discussion
Several similar injuries were found in the literature, but such cases are not common. Therefore, there is no precise consensus on the appropriate actions and timing to achieve better treatment outcomes and reduce the risk of complications. Injuries of this nature are usually caused by high-energy trauma, such as motor vehicle accidents, falls from stairs, or falls from heights [2–6]. In these and similar cases, the impact not only fractures the proximal part of the humerus but also forces the humeral head through all the tissues and ribs into the chest cavity. Even in more common cases such as anterior dislocations, injury to the brachial plexus occurs quite frequently (0.4%) [6], especially in older age groups which have increased risk for tissue damage [7]. Other example would be open anterior dislocations which often result in septic arthritis or necrosis due to impaired blood supply [8]. Compared to these cases, intrathoracic dislocation is way more dangerous as the fragment or part of the humerus can damage blood vessels and nerves while traveling into the chest cavity, resulting in a high risk of neuropathic and circulatory complications. Therefore, it can be considered a “miracle” that there were no neurological complications in this case. Other cases described in the literature include injuries to the subclavian artery, costocervical trunk, or even bone fragments near the aorta [5]. Some cases with neurological complications were found, such as axillary neuropathy, median and ulnar nerve neuropraxia, and secondary brachial plexus injuries. Despite the fact that many of the described patients regained normal blood circulation and nerve function, some experienced incomplete recovery [2–6]. The following treatment principles were similar as they adhere to basic guidelines for these type of traumas. First stabilization of the patient’s condition and respiratory system, extraction of the humeral head, and endoprosthetic replacement of the damaged joint. However, the exact methods of performing these procedures are not clearly defined. Some authors suggest leaving the humeral fragment in the chest cavity if it does not help improving the patient’s condition in the long run, while some suggest that it must always be removed [5]. The precise circumstances and size of the fragment that can be left in the thoracic cavity, as well as the potential consequences of such a decision, remain unclear. Therefore, it is important to document and evaluate the most common complications and treatment methods in order to ensure treatment success.
Conclusions
This clinical case highlights the importance of assessing and treating significant and complex traumas. The treatment priority should be stabilization of the patient’s condition, along with appropriate diagnostic procedures to accurately diagnose and determine the appropriate treatment. Documentation and analysis of such cases are crucial for better understanding these injuries and identifying more effective treatment methods, particularly considering the potential complications. Since this type of trauma is rare, further research and case documentation are necessary to improve their diagnosis and treatment.
Acknowledgements. None.
References
1. Flint JH, Carlyle LM, Christiansen CC, Nepola JV. Case report and literature review anterior shoulder dislocation with three–part proximal humerus fracture and humeral shaft fracture. Iowa Orthop J 2009; 29: 105–113. Available at: <https://pubmed.ncbi.nlm.nih.gov/19742096/>.
2. Frodl A, Eberbach H, Senbaklavaci Ö, Schmal H, Jaeger M. Fracture dislocation of the humerus with intrathoracic humeral head fragment – a case report and review of the literature. Trauma Case Rep 2022; 37: 100592. DOI: 10.1016/j.tcr.2021.100592.
3. Tsai YM, Shen PH, Chang H, Tzao C, Lee SC, Cheng YL. Intrathoracic displacement of a fractured humeral head due to blunt trauma. Ann Thorac Cardiovasc Surg 2014; 20 Suppl: 592–594. DOI: 10.5761/atcs.cr.12.02194.
4. Rupprecht H, Ghidau M, Gaab K. Severe thoracic trauma due to an intrathoracic dislocation of a fractured humeral head in an aged patient; a case report. Bull Emerg Trauma 2017; 5(3): 212–214. Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5547210/>.
5. Chen J, Yan J, Wang S, Zhong H, Zhou H. Intrathoracic dislocation of the humeral head accompanied by polytrauma: How to treat it? Ulus Travma Acil Cerrahi Derg 2015; 21(2): 149–151. DOI: 10.5505/tjtes.2015.72566.
6. Fernández AI, Fernández AG. Intrathoracic fracture – dislocation of the shoulder. J Clin Orthop Trauma 2018; 9(Suppl 2): S54–S57. DOI: 10.1016/j.jcot.2018.04.001.
7. Makovskiy AA, Fedoruk GV, Stepanchenko AP, Dubrov VE. [Comparison of the pattern injuries of the shoulder joint after dislocation in patients different age groups.] Adv Gerontol 2019; 32(1–2): 198–202. Available at: <https://pubmed.ncbi.nlm.nih.gov/31228389/>.
8. Faur CI, Anglitoiu B, Ungureanu AM. Open anterior glenohumeral dislocation with associated supraspinatus avulsion: a case report. World J Clin Cases 2019; 7(7): 849–854. DOI: 10.12998/wjcc.v7.i7.849.7.
9. Tiefenboeck TM, Zeilinger J, Komjati M, Fialka C, Boesmueller S. Incidence, diagnostics and treatment algorithm of nerve lesions after traumatic shoulder dislocations: a retrospective multicenter study. Arch Orthop Trauma Surg 2020; 140(9): 1175–1180. DOI: 10.1007/s00402-020-03348-z.
10. Sola Junior WC, Dos Santos PS. Intrathoracic fracture – dislocation of the humerus – case report and literature review. Rev Bras Ortop 2017; 52(2): 215–219. DOI: 10.1016/j.rboe.2017.01.005.
11. Kappel P, Imach S, Wafaisade A. Intrathoracic fracture dislocation in a patient with proximal humerus fracture. Dtsch Arztebl Int 2021; 118: 578. DOI: 10.3238/arztebl.m2021.0065.