Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2023, vol. 22(3), pp. 173–178 DOI: https://doi.org/10.15388/LietChirur.2023.22(3).7
Pulmonary Vein Occlusion Requiring Lobectomy after Radiofrequency Catheter Ablation for Atrial Fibrillation: A Case Report and Review of the Literature
Žymantas Jagelavičius
Centre of Thoracic Surgery, Clinic of Chest Diseases, Immunology and Allergology, Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
Department of Thoracic Surgery, Centre of Cardiothoracic Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: zymantas.jagelavicius@mf.vu.lt
Ana Baužienė
Department of Thoracic Surgery, Centre of Cardiothoracic Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: ana.bauziene@gmail.com
Vytautas Jovaišas
Department of Thoracic Surgery, Centre of Cardiothoracic Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: vytautas.jovaisas@santa.lt
Ričardas Janilionis
Centre of Thoracic Surgery, Clinic of Chest Diseases, Immunology and Allergology, Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
Department of Thoracic Surgery, Centre of Cardiothoracic Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: richard.janilionis@gmail.com
Abstract. Pulmonary vein stenosis is a potential complication after radiofrequency ablation for atrial fibrillation. We present an unusual case of this complication that progressed to vein occlusion and required lobectomy and review the literature. A 54-year-old man presented with persistent chest pain, dry cough, and hemoptysis. Seven months before he underwent radiofrequency catheter ablation for atrial fibrillation. Chest computed tomography showed a narrowing of the left lower pulmonary vein after the procedure. The patient was treated conservatively. On the presentation, a chest computed tomography scan showed total pulmonary vein occlusion. A quantitative ventilation/perfusion scan revealed no perfusion to the left lower lobe. A balloon angioplasty was performed, however unsuccessfully. The left lower lobectomy was performed. Six years after the lobectomy the patient has neither cardiac nor pulmonary symptoms. Pulmonary vein occlusion after radiofrequency ablation for atrial fibrillation leading to lung resection is still a possible severe complication.
Key words: radiofrequency ablation, pulmonary vein stenosis, pulmonary vein occlusion, lobectomy.
Received: 2023/04/20. Accepted: 2023/06/09.
Copyright © 2023 Žymantas Jagelavičius, Ana Baužienė, Vytautas Jovaišas, Ričardas Janilionis. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Radiofrequency catheter ablation (RFA) is a widely used intervention for paroxysmal atrial fibrillation (AF) treatment. Pulmonary vein stenosis (PVS) is one of the potential complications of RFA for AF and occurs in up to 3% of patients [1]. Percutaneous transcatheter techniques using balloon angioplasty with or without stent implantation have been reported as the standard treatment for symptomatic PVS [1–3]. However, a surgical procedure like lobectomy may be necessary in cases when endovascular treatment fails or if a pulmonary vein is occluded [4]. We report a case of PVS which progressed to pulmonary vein occlusion (PVO) despite conservative management and the attempt of endovascular vein dilation and lead to the left lower lobectomy. We also review the literature of cases when pulmonary resection was performed for PVS or PVO.
Case report
A 54-year-old man was admitted to the Department of General Thoracic Surgery with persistent left pleuritic chest pain, a dry cough that worsened over the preceding two months, and hemoptysis which developed three weeks ago.
The patient previously suffered from AF which was difficult to control with oral drugs. A successful RFA procedure was performed seven months before the admission, and the sinus rhythm was restored. However, chest computed tomography (CT), performed the next day after RFA, showed a significant narrowing of the left lower pulmonary vein (up to 3.5 mm) (Figure 1A). The patient had only mild symptoms and was treated conservatively.
On admission a chest X-ray showed subtle patchy consolidations in the left lower lobe of the lung (Figure 1B). A chest CT scan showed patchy consolidations, areas of atelectasis of the left lower lobe parenchyma (Figure 1C), and the absence of communication between the left lower pulmonary vein and the left atrium (Figure 1D). A quantitative ventilation/perfusion scan (99mTc-MAA 98MBq) revealed that the left lung was receiving only 15% of the overall lung perfusion with no perfusion to the left lower lobe (Figure 2). Bronchoscopy found striking hyperemia and brisk bleeding to touch of the mid and distal left lower lobe bronchus. Based on instrumental and clinical findings, it was decided to perform balloon angioplasty with further stent implantation. However, the procedure was unsuccessful, due to an invisible lumen or dimple, that can be probed in the vein.
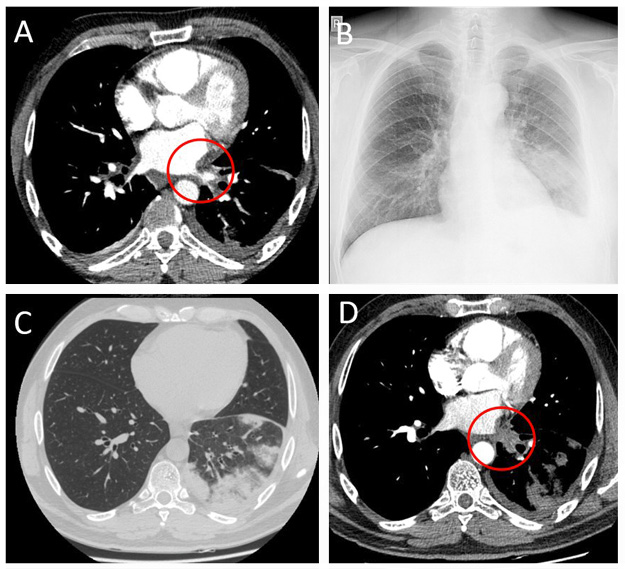
Figure 1. CT scan showing narrowing of the left lower PV (A); chest X-ray with patchy area in the left lower lobe (B); CT scan showing areas of patchy consolidation of the left lower lobe (C), and total occlusion of the left lower PV (D)
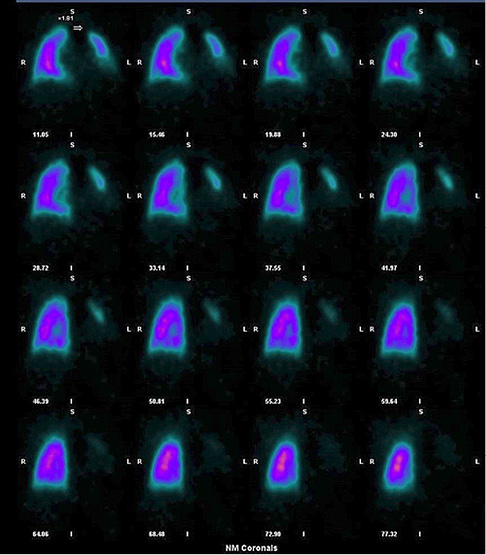
Figure 2. Quantitative ventilation/perfusion scan
The patient underwent a left lower lobectomy thereafter. Upon exploration 500 ml of cloudy serohemorrhagic fluid was found in the left pleural cavity. The lower lobe was extremely dense and firm. There were chronic inflammatory adhesions to the chest wall, diaphragm and pericardium. Numerous tiny sinuous collateral vessels were tracking from the left lower lobe across the fissure to the upper lobe and around the bronchus toward the hilum. The lower pulmonary vein was completely obliterated. The final pathological examination confirmed total obliteration of the lower pulmonary vein and foci of atelectasis, extensive areas of necrosis, and hemorrhages in the pulmonary tissue.
The postoperative course was uneventful. Six years follow-up the patient has neither cardiac nor pulmonary symptoms.
Discussion
Pulmonary vein stenosis or even occlusion after RFA is a rare, however severe, and often underdiagnosed complication. The incidence of PVS after RFA in recent years is decreasing due to modern ablation techniques and varies from 0% to 3% [1, 2, 5–7]. However, with the increasing numbers of AF and RFA procedures some patients are still at risk.
Although the main treatment for symptomatic and significant PVS or even PVO is an endovascular angioplasty procedure, there might be cases when this treatment fails or irreversible changes in lung parenchyma develop [1, 2, 7, 8]. In such cases, lung resection may be necessary. Reviewing the literature, we have found 11 cases of PVS or PVO after RFA that required lung resection (Table 1) and compared to our case [4, 9–18]. There was one more case in which lobectomy was attempted, but because of fibrothorax and dense adhesions not performed [19]. Schoene et al. [20] recently described a surgical pulmonary vein angioplasty case, which might be another option for the surgical treatment of PVS. However, if the case is already chronic with irreversible changes in the lung parenchyma, this procedure would not be helpful.
Table 1. Analysis of PVS and PVO cases after RFA for AF which required lung resection
|
Author |
Yang et al. [9] |
Nehra et al. [10] |
Libretti et al. [4] |
Steliga et al. [11] |
Lee et al. [12] |
Lo et al. [13] |
Cheng et al. [14] |
Lopez-Reyes et al. [15] |
Papakonstantinou et al. [16] |
Xuan et al. [17] |
Matsumoto et al. [18] |
Recent case |
|
Year |
2007 |
2009 |
2010 |
2010 |
2015 |
2016 |
2018 |
2018 |
2018 |
2020 |
2021 |
2023 |
|
Age |
57 |
58 |
17 |
51 |
60 |
47 |
37 |
57 |
50 |
38 |
48 |
54 |
|
Sex |
Male |
Female |
Male |
Female |
Male |
Female |
Male |
Male |
Male |
Male |
Male |
Male |
|
The time between |
1 month |
24 months |
Few |
2 months |
12 months |
6 months |
12 months |
6 months |
8 months |
2 weeks |
36 months |
1 day (PVS), 7 months (PVO) |
|
Type of PV obstruction before surgery |
PVO |
PVO |
PVO |
PVO |
PVS |
PVO |
PVO |
PVT |
PVO |
PVO |
PVS |
PVO |
|
Which PV |
All 4 |
LU, LL |
LL |
LU |
LU, LL |
RL |
LU |
LU |
LU |
LU |
LL |
LL |
|
V/Q scan |
No data |
0% to the left lung |
No data |
24% to the left lung and 0% to the LU lobe |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
15% to the left lung and 0% to the LL lobe |
|
Interventional treatment before surgery (number of attempts) |
Surgical pericardial patch enlargement, (1), balloon dilation and stenting (3) |
No |
Balloon dilation (3) |
No |
Bronchial angiography (1), stenting (1) |
No |
Bronchial artery embolization (1) |
No |
Diagnostic wedge resection (1) |
Bronchial artery embolization (2) |
Bronchial artery embolization (2) |
Balloon dilation and stenting (1) |
|
The time between the last RFA and pulmonary resection |
26 months |
36 months |
12 months |
6 months |
24 months |
6 months |
12 months |
7 months |
8 months |
2 weeks |
44 months |
8 months |
|
Indications for pulmonary resection |
Hemoptysis, PVO |
Hemoptysis, PVO of both left PVs |
Recurrent pneumonia, PVO |
Progressive symptoms, PVO |
Hemoptysis, PV rupture |
Hemoptysis, progressive symptoms, PVO |
Hemoptysis, PVO |
Hemoptysis, progressive PVT |
Hemoptysis, PVO |
Hemoptysis |
Hemoptysis, uncontrolled AF |
Hemoptysis, PVO |
|
Type of resection |
LLL |
LP |
LLL |
LUL |
LP |
RLL (VATS) |
LUL (VATS) |
LUL |
LUL |
LUL |
LLL |
LLL |
|
Symptoms reduction after surgery |
Yes |
No data |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
AF after all |
No AF |
No data |
No AF |
Persist |
No data |
No AF |
No AF |
No AF |
No AF |
No data |
No AF |
No AF |
PVS – pulmonary vein stenosis, PVO – pulmonary vein occlusion, RFA – radiofrequency ablation, PV – pulmonary vein, PVT – pulmonary vein thrombosis, LU – left upper, LL – left lower, RL – right lower, AF – atrial fibrillation, LUL – left upper lobectomy, LLL – left lower lobectomy, LP – left pneumonectomy, RLL – right lower lobectomy, VATS – video-assisted thoracic surgery.
The course of PVS usually is an unpredictable process according to the degree and the time. It may progress or even partially resolve [1]. Symptoms mostly are nonspecific (dyspnea, cough, chest pain, pneumonia). However, analyzing indications for surgery, it is noticeable that most of the patients suffered from persistent hemoptysis. The time of symptoms varies widely; however, they usually start sometime (at least 1 month) after RFA. In all cases, symptoms progressed and hemoptysis developed. In our case PVS was diagnosed right after RFA, nevertheless, symptoms at the beginning were very mild and controlled with drugs. However, the disease progressed to PVO with irreversible changes in the lung parenchyma.
A radiological examination may show only some non-specific abnormalities such as pulmonary infiltrates or pleural effusion, therefore specific visualization of the pulmonary vein is always necessary to confirm the diagnosis [1, 2]. A V/Q scan could be an important tool to assess the severity of stenosis [8]. In analyzed cases, diagnosis of PVS or PVO was usually confirmed by imaging techniques. In eight out of 11 cases, as well as in ours, a total PVO was confirmed. Total PV thrombosis was found in one case, and in two cases, severe PVS. However, a V/Q scan showing a significant reduction of lung perfusion was performed only in two previous cases.
Before the surgery endovascular treatment was applied only in three cases. It could be explained that in most cases, a total PVO was diagnosed and a long time passed after the RFA. Permanent symptoms, such as hemoptysis, and probably irreversible changes in lung parenchyma were already developed. In such cases, it is difficult to expect the success of endovascular management. Interestingly, there were four cases in which bronchial angiography and embolization were attempted, however, without significant improvement. In our case, an unsuccessful endovascular procedure was attempted seven months after RFA when total PVO was already noticeable.
The time of surgery after the last RFA procedure varies widely. It shows how different could be the development of PVO. Although PVS after RFA may involve several PVs, PVO was usually detected in a single vein (9 of 11 cases). These cases lead to lobectomies as well as ours. Only two cases described irreversible lesions of both left-sided PVs, in which left pneumonectomies were performed. Most of the cases had lesions on the left side, and there was no predominance between the upper or lower vein. After the surgery, a significant reduction of symptoms was achieved, and AF was usually successfully managed before. Our case was not an exception.
Conclusion
Severe complication after RFA for AF leading to total PVO and lung resection is still possible. The angioplasty procedure should be performed without delay in the symptomatic patient with PVS.
Disclosure statement
The authors have no conflict of interest. Informed consent was obtained from the patient.
References
1. Rostamian A, Narayan SM, Thomson L, Fishbein M, Siegel RJ. The Incidence, Diagnosis, and Management of Pulmonary Vein Stenosis as a Complication of Atrial Fibrillation Ablation. J Interv Card Electrophysiol 2014; 40(1): 63–74.
2. Holmes DR Jr, Monahan KH, Packer D. Pulmonary Vein Stenosis Complicating Ablation for Atrial Fibrillation: Clinical Spectrum and Interventional Considerations. JACC Cardiovasc Interv 2009; 2(4): 267–276.
3. Pazos-López P, García-Rodríguez C, Guitián-González A, Paredes-Galán E, Álvarez-Moure MAG, Rodríguez-Álvarez M, Baz-Alonso JA, Teijeira-Fernández E, Calvo-Iglesias FE, Íñiguez-Romo A. Pulmonary Vein Stenosis: Etiology, Diagnosis and Management. World J Cardiol 2016; 8(1): 81–88.
4. Libretti L, Ciriaco P, Zannini P. Pulmonary Vein Stenosis Requiring Lobectomy after Radiofrequency Catheter Ablation for Atrial Fibrillation. J Cardiovasc Surg (Torino) 2012; 53(6): 821–823.
5. Gupta A, Perera T, Ganesan A, Sullivan T, Lau DH, Roberts-Thomson KC, Brooks AG, Sanders P. Complications of Catheter Ablation of Atrial Fibrillation: A Systematic Review. Circ Arrhythm Electrophysiol 2013; 6(6): 1082–1088.
6. Baman T, Latchamsetty R, Oral H. Complications of Radiofrequency Catheter Ablation for Atrial Fibrillation. J Atr Fibrillation 2011; 4(3): 345.
7. Schoene K, Arya A, Jahnke C, Paetsch I, Nedios S, Hilbert S, Bollmann A, Hindricks G, Sommer P. Acquired Pulmonary Vein Stenosis after Radiofrequency Ablation for Atrial Fibrillation: Single-Center Experience in Catheter Interventional Treatment. JACC Cardiovasc Interv 2018; 11(16): 1626–1632.
8. Fender EA, Widmer RJ, Hodge DO, Cooper GM, Monahan KH, Peterson LA, Holmes DR Jr, Packer DL. Severe Pulmonary Vein Stenosis Resulting From Ablation for Atrial Fibrillation: Presentation, Management, and Clinical Outcomes. Circulation 2016; 134(23): 1812–1821.
9. Yang HM, Lai CK, Patel J, Moore J, Chen PS, Shivkumar K, Fishbein MC. Irreversible Intrapulmonary Vascular Changes after Pulmonary Vein Stenosis Complicating Catheter Ablation for Atrial Fibrillation. Cardiovasc Pathol 2007; 16(1): 51–55.
10. Nehra D, Liberman M, Vagefi PA, Evans N, Inglessis I, Kradin RL, Ono J, Kanarek DJ, Gaissert HA. Complete Pulmonary Venous Occlusion after Radiofrequency Ablation for Atrial Fibrillation. Ann Thorac Surg 2009; 87(1): 292–295.
11. Steliga MA, Ghouri M, Massumi A, Reul RM. Lobectomy for Pulmonary Vein Occlusion Secondary to Radiofrequency Ablation. J Cardiovasc Electrophysiol 2010; 21(9): 1055–1058.
12. Lee JY, Chon GR, Park JH, Kang BJ, Shim TS, Jo KW. Massive Hemoptysis Due to Pulmonary Vein Stenosis Following Catheter Ablation for Atrial Fibrillation. Respir Care 2015; 60(3): e52–55.
13. Lo CM, Lu HI, Chen YY, Chang JP. Thoracoscopic Lobectomy for Pulmonary Vein Occlusion after Radiofrequency Catheter Ablation of Atrial Fibrillation. J Cardiothorac Surg 2016; 11: 12.
14. Cheng S, Lu X, Wang J, Liu T, Zhang X. Thoracoscopic Lobectomy for Massive Hemoptysis Caused by Complete Pulmonary Vein Occlusion after Radiofrequency Ablation for Atrial Fibrillation. J Thorac Dis 2018; 10(4): E296–E300.
15. López-Reyes R, García-Ortega A, Torrents A, Feced L, Calvillo P, Libreros-Niño EA, Escrivá-Peiró J, Nauffal D. Pulmonary Venous Thrombosis Secondary to Radiofrequency Ablation of the Pulmonary Veins. Respir Med Case Rep 2018; 23: 46–48.
16. Papakonstantinou NA, Zisis C, Kouvidou C, Stratakos G. Lobectomy Due to Pulmonary Vein Occlusion after Radiofrequency Ablation for Atrial Fibrillation. Korean J Thorac Cardiovasc Surg 2018; 51(4): 290–292.
17. Xuan Z, Liu B, Ci M, Wang Z, Fan Y. Hemoptysis Secondary to Pulmonary Vein Stenosis after Radiofrequency Ablation for Atrial Fibrillation: A Case Report and Literature Review. J Interv Med 2020; 3(2): 98–100.
18. Matsumoto S, Suzuki M, Matsubayashi S, Tsukada A, Kusaba Y, Katsuno T, Iikura M, Izumi S, Takeda Y, Hojo M, Sugiyama H. Refractory Hemoptysis Caused by Severe Pulmonary Vein Stenosis after Multiple Catheter Ablations. Intern Med 2021; 60(20): 3279–3284.
19. O’Gorman KJ, Sjulin TJ, Bowen DK, Morris MJ. The Use of Lobectomy for Management of Clinically Significant Pulmonary Vein Stenosis and Occlusion Refractory to Percutaneous Intervention. Respir Med Case Rep 2019; 26: 321–325.
20. Schoene K, Sommer P, Arya A, Kostelka M, Mohr FW, Misfeld M, Vollroth M, Bollmann A, Lurz J, Hindricks G, Seeburger J. Complex Cases of Acquired Pulmonary Vein Stenosis after Radiofrequency Ablation: Is Surgical Repair an Option? Europace 2019; 21(1): 73–79.