Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(1), pp. 40–44 DOI: https://doi.org/10.15388/LietChirur.2024.23(1).5
An Unusual Case of Cheiralgia Paresthetica Caused by Lipoma
Tomas Mačiulaitis
Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: tomas.maciulaitis@mf.stud.vu.lt
Aira Jucaitytė
Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: jucaityteaira@gmail.com
Mindaugas Minderis
Center of Plastic and Reconstructive Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: mminderis@gmail.com
Abstract. Cheiralgia paresthetica (CP) is a distinctive clinical condition arising from the compression of the superficial branch of the radial nerve (SBR). Typically, CP manifests as a burning-type pain in the dorsal and radial aspect of the hand. Existing literature highlight various etiological factors contributing to this condition, including constriction of the wrist, as with tight wristwatches or handcuffs. Symptoms may also arise from blunt traumas, distal radius fractures, and iatrogenic causes. However, CP induced by a lipoma is an exceptionally rare phenomenon. In this context, we present a case exemplifying the diagnosis and management of lipoma-induced CP.
Keywords: Cheiralgia paresthetica, superficial radial nerve, lipoma, pseudolipoma.
Neįprastas klinikinis atvejis: lipomos sąlygota Cheiralgia paresthetica
Santrauka. Cheiralgia paresthetica (CP) – reta patologija, kurią sukelia paviršinio stipininio nervo kompresija. Įprastai CP kliniškai būdingas skausmingas deginimo pojūtis, lokalizuotas nugarinės ir stipininės plaštakos dalių projekcijoje. Mokslinėje literatūroje nurodoma įvairių šiai ligai būdingų etiologinių veiksnių. Dažniausiai tai veiksniai, provokuojantys veržimą riešo srityje, pavyzdžiui, antrankiai ar ankšti riešo srities aksesuarai. Simptomų taip pat gali sukelti stipinkaulio distalinio galo lūžiai, bukos traumos ar jatrogeniniai pažeidimai. Straipsnyje dalijamasi patirtimi diagnozuojant ir gydant lipomos sąlygotą CP. Lipoma – atipinė ir itin reta CP priežastis.
Reikšminiai žodžiai: Cheiralgia paresthetica, paviršinis stipininis nervas, lipoma, pseudolipoma.
Received: 2023/12/18. Accepted: 2024/01/02.
Copyright © 2024 Tomas Mačiulaitis, Aira Jucaitytė, Mindaugas Minderis. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
The superficial branch of the radial nerve (SBR) is a terminal radial nerve sensory branch. It is located lateral to the radial artery, beneath the brachioradialis muscle, piercing the deep fascia at the lower third of the forearm where it lies superficial underneath the skin. Due to SBR’s anatomical location, the nerve is highly vulnerable to trauma and compression [1]. Cheiralgia paresthetica (CP) was first described by Wartenberg in 1932 as a mononeuropathy, defined by compression of the SBR [2]. The condition presents itself as pain and paresthesia located on the dorsal and radial aspect of the hand [3]. Lipomas of the distal forearm are an uncommon cause of CP [4]. Due to its rare occurrence, we report a case of SBR compression by lipoma in an otherwise healthy male.
Case report
A 66-year-old male patient was referred to our center due to a six-month history of pain and paresthesia in the dorsal and distal aspect of the right forearm.

Figure 1. Palpable mass located at the distal forearm

Figure 2. Post-trauma scar
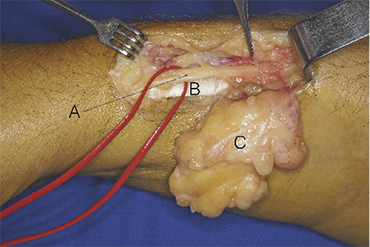
The patient had a history of a penetrating trauma in the relevant area during childhood. In addition, the patient emphasized a slowly enlarging palpable lesion which occurred in concert with the presented symptoms. Physical examination demonstrated a palpable mass beneath the distal part of the scar (Figures 1, 2).
Sonoscopy revealed a non-encapsulated mass, measuring 6 cm at its largest diameter (Figure 3).
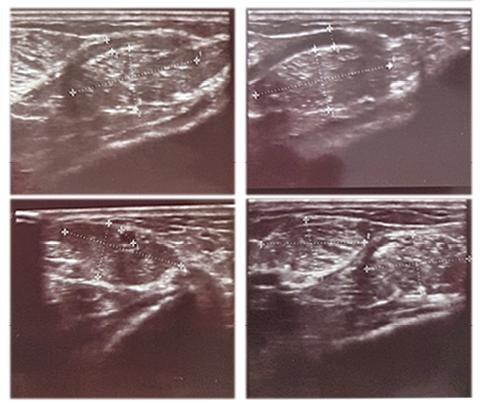
Figure 3. Ultrasound image of the lesion
The exact position of the lesion coincides with the anatomical location where SBR, piercing the deep fascia, approaches the subcutaneous layer. The mass was extirpated and confirmed to be a lipoma (Figures 4, 5).
|
|
|
|
Figure 4. Forearm. A – superficial radial nerve; B – brachioradial tendon, C – lipoma. |
Figure 5. 6×4 cm excised tumor |
Decompressive fasciotomy reaching the extensors pelvis was also performed.
Following a two-week postoperative period, the patient attended a consultation, noting the alleviation of symptoms.
Discussion
Cheiralgia paresthetica is a relatively rare condition when compared to other nerve compression syndromes [5]. The challenge for medical practitioners lies in diagnosing and discerning this uncommon condition, particularly given the elusive nature of the annual incidence rate.
Various iatrogenic factors have been reported as potential contributors to CP among them surgical interventions such as K-wire fixation during distal radial fracture management and interventions like local steroid injections [6, 7]. Additionally, CP has been associated with procedures like peripheral vein cannulation [8]. Acknowledging the susceptibility of the SBR to iatrogenic influences, a thorough understanding of its anatomy emerges as essential for both prevention and effective management.
|
|
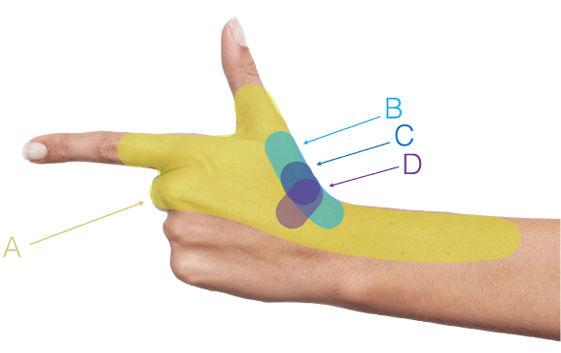
Figure 6. Visual representation of differential pain localization in various hand and wrist pathologies A – CP, B – De Quervain’s tenosynovitis, C – rhizarthrosis, D – schaphotrapeziotrapezoid arthritis. |
The hand and wrist region is notably complex, housing a wide array of specific pathologies. Many of these conditions present with similar symptoms, often resulting in misdiagnoses of CP. De Quervain’s tenosynovitis, for instance, is characterized by inflammation, causing localized pain, swelling, and impaired thumb mobility [9]. Similarly, Flexor carpi radialis tendinitis, driven by tendon inflammation, produces localized pain and tenderness, especially during wrist movements [10]. Scaphotrapeziotrapezoid arthritis signifies the degeneration of the wrist’s scaphotrapeziotrapezoid joint, located near the base of the thumb, and results in pain, exacerbated by activities involving gripping or twisting motions [11]. The primary distinguishing feature of CP is the presence of diffuse pain, along with sensory deficits, specifically localized in the radial aspect of the forearm. This distinction sets it apart from other conditions. Here, we provide an illustration depicting the differential localization of pain in various hand and wrist pathologies, as well as in CP (Figure 6).
In our case, we contemplate the possibility of the CP-induced lipoma originating as a “pseudolipoma”/“posttraumatic lipoma” – a hypothesis stemming from existing literature. Some lipomas are thought to have a posttraumatic origin linked to prior blunt soft tissue injuries [12]. The idea that soft tissue trauma could lead to the protrusion of adipose tissue through Scarpa’s fascia, forming pseudotumors in fatty tissues, was first introduced in 1969 [13]. Another perspective proposes the formation of lipomas as a consequence of preadipocyte differentiation and proliferation, driven by the release of cytokines following soft tissue trauma and hematoma formation [14, 15].
The literature does highlight associations between soft tissue trauma and lipoma formation, as exemplified by Aust et al. [12]. The study, involving 19 patients, revealed the detection of lipomas near the trauma site, with an average time interval of approximately 2 to 6 years after the trauma. However, Nigri et al. [16] reported a case of a substantial inframuscular lipoma occurring as long as 14 years following a blunt trauma event.
With a significant 50-year gap between the initial trauma and the emergence of the lipoma in our case, it appears increasingly improbable that the lipoma should not be categorized as a pseudolipoma. This extended time frame suggests that the lipoma’s development may have been more coincidental rather than directly tied to the past trauma.
Conclusions
Attention is drawn to a rare and poorly appreciated condition of the CP causing sensory neuropathy. In our case, surgical enucleation of the compressing factor, lipoma, along with decompressive fasciotomy resulted in full recovery from the sensory symptoms and improvement in the quality of life.
Informed consent. Written informed consent was obtained from a legally authorized representative(s) for anonymized patient information to be published in this article.
Declaration of conflicting interests. The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding. The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
1. Shields LBE, Iyer VG, Zhang YP, Shields CB. Etiological study of superficial radial nerve neuropathy: series of 34 patients. Front Neurol 2023; 14: 1175612. DOI: 10.3389/fneur.2023.1175612.
2. Wartenberg R. Cheiralgia paraesthetica (Isolierte Neuritis des Ramus superficialis nervi radialis). Zeitschrift für die gesamte Neurologie und Psychiatrie 1932; 141: 145–155. DOI: 10.1007/BF02909851.
3. Jacobson JA, Fessell DP, Lobo Lda G, Yang LJ. Entrapment neuropathies I: upper limb (carpal tunnel excluded). Semin Musculoskelet Radiol 2010; 14(5): 473–486. DOI: 10.1055/s-0030-1268068.
4. Phalen GS, Kendrick JI, Rodriguez JM. Lipomas of the upper extremity. A series of fifteen tumors in the hand and wrist and six tumors causing nerve compression. Am J Surg 1971; 121(3): 298–306. DOI: 10.1016/0002-9610(71)90208-x.
5. da Costa JT, Baptista JS, Vaz M. Incidence and prevalence of upper-limb work related musculoskeletal disorders: a systematic review. Work 2015; 51(4): 635–644. DOI: 10.3233/WOR-152032.
6. Singh S, Trikha P, Twyman R. Superficial radial nerve damage due to Kirschner wiring of the radius. Injury 2005; 36(2): 330–332. DOI: 10.1016/j.injury.2004.04.017.
7. Chodoroff G, Honet JC. Cheiralgia paresthetica and linear atrophy as a complication of local steroid injection. Arch Phys Med Rehabil 1985; 66(9): 637–639.
8. Thrush DN, Belsole R. Radial nerve injury after routine peripheral vein cannulation. J Clin Anesth 1995; 7(2): 160–162. DOI: 10.1016/0952-8180(94)00029-4.
9. Wolf JM, Sturdivant RX, Owens BD. Incidence of de Quervain’s tenosynovitis in a young, active population. J Hand Surg Am 2009; 34(1): 112–115. DOI: 10.1016/j.jhsa.2008.08.020.
10. Larsen CG, Fitzgerald MJ, Nellans KW, Lane LB. Management of de Quervain tenosynovitis: a critical analysis review. JBJS Rev 2021; 9(9): e21.00069. DOI: 10.2106/JBJS.RVW.21.00069.
11. Catalano 3rd LW, Ryan DJ, Barron OA, Glickel SZ. Surgical management of scaphotrapeziotrapezoid arthritis. J Am Acad Orthop Surg 2020; 28(6): 221–228. DOI: 10.5435/JAAOS-D-19-00539.
12. Aust MC, Spies M, Kall S, Jokuszies A, Gohritz A, Vogt P. Posttraumatic lipoma: fact or fiction? Skinmed 2007; 6(6): 266–270. DOI: 10.1111/j.1540-9740.2007.06361.x.
13. Brooke RI, MacGregor AJ. Traumatic pseudolipoma of the buccal mucosa. Oral Surg Oral Med Oral Pathol 1969; 28(2): 223–225. DOI: 10.1016/0030-4220(69)90290-4.
14. Signorini M, Campiglio GL. Posttraumatic lipomas: where do they really come from? Plast Reconstr Surg 1998; 101(3): 699–705. DOI: 10.1097/00006534-199803000-00017.
15. Copcu E, Sivrioglu NS. Posttraumatic lipoma: analysis of 10 cases and explanation of possible mechanisms. Dermatol Surg 2003; 29(3): 215–220. DOI: 10.1046/j.1524-4725.2003.29052.x.
16. Nigri G, Dente M, Valabrega S, Beccaria G, Aurello P, D’Angelo F, Di Marzo F, Ramacciato G. Giant inframuscular lipoma disclosed 14 years after a blunt trauma: a case report. J Med Case Reports 2008; 2: 318. DOI: 10.1186/1752-1947-2-318.