Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(1), pp. 18–24 DOI: https://doi.org/10.15388/LietChirur.2024.23(1).3
Bedside Teaching in Undergraduate Surgical Education: A Pilot Study of Students’ Perspective
Mohammed Alfehaid
Department of Surgery, Unaizah College of Medicine and Medical Sciences, Qassim University, Unaizah, Saudi Arabia
E-mail: M.alfehaid@qu.edu.sa
Abstract. Background. Bedside teaching is an important tool in medical education. In recent years, studies have shown that this tool has witnessed gradual deterioration due to various reasons. Hence this pilot study was conducted to assess the students’ perspective about this tool and suggest remedies for the deficiencies. Methodology. An anonymous questionnaire was designed and students were requested to register the response offline. Data was analysed and inferences made. Results. Various deficiencies were highlighted by the students that require correction and improvement. Unavailability of suitable patients is a significant barrier. Communication skills and understanding of infection control protocols had got improved in 84% and 94% students respectively. Half of the students were fully satisfied or satisfied with the overall conduct of the bedside teaching and the other half were either partially satisfied or dissatisfied. Conclusion. There is a need to improve bedside teaching in Undergraduate Surgery course. Simulation sessions need to be devised and enhanced. Faculty development sessions to train the teachers are required.
Keywords: bedside teaching, simulation, communication skills, infection control.
Received: 2023/09/22. Accepted: 2023/10/30.
Copyright © 2024 Mohammed Alfehaid. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Bedside teaching (BST) is a component of medical education where teaching occurs in the presence of a patient in the hospital setting, or else the office or long-term care facility [1, 2]. It is a vital component of medical education and considered as one of the reliable tools to develop clinical and communication skills [3, 4].
Sylvius (1614–1672), a renowned French practitioner, was one of the first to record his understanding about the practice and concept of teaching the students during conduct of rounds. He would assert that in order to guide the students toward perfect medical practice, it was essential to encourage them to see patients every day and report back with their observations, thoughts and perceptions related to the patients’ illness and the principles of treatment [1]. Sir William Osler (1849–1920), a renowned clinician-teacher, putting great emphasis on the significance of bedside teaching had stated that to study the phenomena of disease without books is to sail an uncharted sea, whilst to study books without patients is analogous to not to go to sea at all [5–6].
Teaching in front of the patients provides students with opportunities to learn more about the patients using practically all of their senses, including hearing, vision, smell, and touch, as compared to mere listening to a lecture or reading from the notes. Many abilities, notably the humanistic components of medicine, cannot be acquired in a traditional classroom setting [1, 7].
In spite of such importance and historical support for bedside teaching, in recent years, concerns have been raised about a steady decline of BST and various remedies have been suggested [8, 9]. But despite recent innovations to improve practical clinical learning, recent studies have shown that a large proportion of newly qualified doctors have a feeling of being unprepared when transitioning to clinical practice and the unpreparedness is related to a lack of meaningful clinical training during the undergraduate course [10–11].
In the Surgery block of the undergraduate course at the Unaizah College of Medicine, Qassim University, Saudi Arabia, bedside clinical teaching sessions are conducted regularly at King Saud Hospital, Unaizah, which is a secondary level health care facility. But there has been no previous study to analyse this teaching tool ever since it was commissioned in 2012 though such studies have been conducted in other medical colleges in the kingdom [12–13]. It was against this background, that the current study was undertaken as a pilot project, to assess the weaknesses and strengths of the bedside teaching from students’ perspective.
Materials & methods
Study design. An observational descriptive cross-sectional study.
Sampling, sample size estimation and defining the study population. Convenience sampling technique was adopted and the fourth-year (Phase 2, Clinical MD3) medical students undergoing General Surgery clerkship at the Department of Surgery, Unaizah College of Medicine, Qassim University, KSA, were explained the objectives of the study and the ones who voluntarily agreed to enter the study, were enrolled.
Execution. A brief structured questionnaire (Table 1) was designed after adaptation and validation of the concepts from the previously published peer-reviewed studies. That tool was then used to assess the students’ feedback related to their feelings about their bedside teaching venue, satisfaction levels with this mode of education, and the confidence level attained in history-taking, physical examination skills, communication skills infection control protocols. Three-point Likert scale was used to assess the responses except for the overall satisfaction level for which five-point scale was applied. There was one open ended question seeking the suggestions for improvement of bedside teaching in future and the responses to that question were summarized using a thematic approach.
Data Analysis
In this descriptive cross-sectional study, the data were first cleaned and checked for completeness to eliminate any possible errors using the Microsoft Excel 2019 and analyzed by Statistical Product and Service Solutions (SPSS Version 27). Qualitative data was expressed as frequency and proportions. Graphs and tables were used for depiction. Open-ended questions were analyzed using thematic approach. T-test was used to assess the difference in confidence levels between various skills and p value of less than 0.05 was selected as significant.
Ethical Considerations. The study was approved by the departmental ethics committee. Confidentiality of the subjects was maintained by making the questionnaire anonymous and coded.
Results. A total of 25 male students of Phase 2, MD 3 class participated in the study and registered their responses as depicted in Table 1. Only 9 students (36%) and 7 students (28%) felt that bedside teaching disturbs that patient or staff respectively. Majority of the students (≥84%) expressed that there was inadequate number and variety of patients for teaching sessions though 76% (n = 19) found the patients to be cooperative. Overall, at the end of the course, only 48% students felt to be overall highly confident or confident in history taking skills and lack of confidence was most worrisome, in history related to disorders of scrotum (84%) and anorectum (88%). In comparison, confidence levels were significantly higher (p ≤ 0.05) in history taking in gastrointestinal disorders (84%) and hernia (76%). In physical examination skills, 56.9% felt highly confident or else confident but like in history taking, there is a significant difference (p ≤ 0.05) between examination skills of various parts, with lack of confidence levels in scrotal examination, anorectal examination and trauma. At the end of the course, 84% and 94% students felt highly confident or confident in communication skills and infection control respectively.
Table 1. Questionnaire to study the students’ perspective about bedside teaching in Surgery block
|
Do bedside teaching sessions disturb: |
Yes |
No |
Not sure |
|
the privacy and comfort of the patient? |
9 (36%) |
12 (48%) |
4 (16%) |
|
the working of the hospital staff? |
7 (28%) |
11 (44%) |
8 (32%) |
|
Availability and attitude of the patients |
Yes |
No |
Not sure |
|
There was an adequate number of patients. |
3 (12%) |
21 (84%) |
1 (4%) |
|
There was an adequate variety of patients. |
2 (8%) |
22 (88%) |
1 (4%) |
|
Patients were mostly cooperative and displayed positive attitude. |
19 (76%) |
3 (12%) |
3 (12%) |
|
Patients were mostly postoperative, with no relevant clinical findings. |
18 (72%) |
2 (8%) |
5 (20%) |
|
At the end of the course, my confidence level in history taking of patients reporting with complaints related to: |
Highly confident |
Confident |
Not confident |
|
Gastrointestinal system |
11 (44%) |
10 (40%) |
4 (16%) |
|
Urinary system |
1 (4%) |
8 (32%) |
16 (64%) |
|
Thyroid |
6 (24%) |
5 (20%) |
14 (56%) |
|
Lump |
9 (36%) |
7 (28%) |
9 (36%) |
|
Breast |
5 (20%) |
8 (32%) |
12 (48%) |
|
Scrotum |
1 (4%) |
3 (12%) |
21 (84%) |
|
Anorectum |
1 (4%) |
2 (8%) |
22 (88%) |
|
Ulcer |
6 (24%) |
9 (36%) |
10 (40%) |
|
Hernia |
9 (36%) |
10 (40%) |
6 (24%) |
|
Trauma |
4 (16%) |
5 (20%) |
16 (64%) |
|
Confidence level percentage for all (n = 10) the skills in history taking |
21.2% |
26.8% |
52% |
|
At the end of the course, my confidence level in physical examination of: |
Highly confident |
Confident |
Not confident |
|
Abdomen |
17 (68%) |
5 (20%) |
3 (12%) |
|
Thyroid |
11 (44%) |
9 (36%) |
5 (20%) |
|
Lump |
6 (24%) |
11 (44%) |
8 (32%) |
|
Breast |
8 (32%) |
8 (32%) |
9 (36%) |
|
Scrotum |
1 (4%) |
2 (8%) |
22 (88%) |
|
Anorectum |
1 (4%) |
5 (20%) |
19 (76%) |
|
Ulcer |
9 (36%) |
8 (32%) |
8 (32%) |
|
Hernia |
9 (36%) |
9 (36%) |
7 (28%) |
|
Trauma |
3 (12%) |
6 (24%) |
16 (64%) |
|
Confidence level percentage for all (n = 9) the skills in physical examination |
28.9% |
28% |
43.1% |
|
At the end of the course, my confidence level in communication skills: |
Highly confident |
Confident |
Not confident |
|
18 (72%) |
3 (12%) |
4 (16%) |
|
|
At the end of the course, my confidence level in infection control protocols: |
Highly confident |
Confident |
Not confident |
|
13 (52%) |
10 (40%) |
2 (8%) |
|
|
My overall impression about bedside training in Surgery Course |
Effective |
Ineffective |
Not sure |
|
8 (32%) |
9 (36%) |
8 (32%) |
|
Satisfaction level about teaching sessions |
Fully |
Satisfied |
Partially |
Dissatisfied |
Not sure |
|
Academic atmosphere of training place |
5 (20%) |
7 (28%) |
11 (44%) |
2 (8%) |
– |
|
Duration of the training course |
5 (20%) |
4 (16%) |
3 (12%) |
13 (52%) |
– |
|
Duration of each training session |
5 (20%) |
9 (36%) |
3 (12%) |
7 (28%) |
1 (4%) |
|
Approach to common surgical diseases |
7 (28%) |
6 (24%) |
5 (20%) |
7 (28%) |
– |
|
Group size (the number of students in each session) |
15 (64%) |
8 (32%) |
2 (8%) |
– |
– |
|
Course planning (objectives, definite reference) |
5 (20%) |
11 (44%) |
5 (20%) |
3 (12%) |
1 (4%) |
|
Instructors’ teaching approach |
8 (32%) |
7 (28%) |
6 (24%) |
4 (16%) |
– |
|
Overall satisfaction level percentage for all the variables (n = 7) |
28.6% |
29.7% |
20% |
20.6% |
1.1% |
|
Suggestions for improvement of bedside training 1. Practice with simulated patients before actually starting bedside teaching with real patients (n = 7, 28%). 2. To conduct bedside sessions in second half of the Surgery Course when students have already attended theoretical lectures/attended team-based learning sessions related to most common surgical disorders, so that the students are more confident due to better understanding of the diseases (n = 6, 24%). |
|||||
The overall satisfaction level for the way the bedside teaching activity was organised are as depicted in Figure 1.
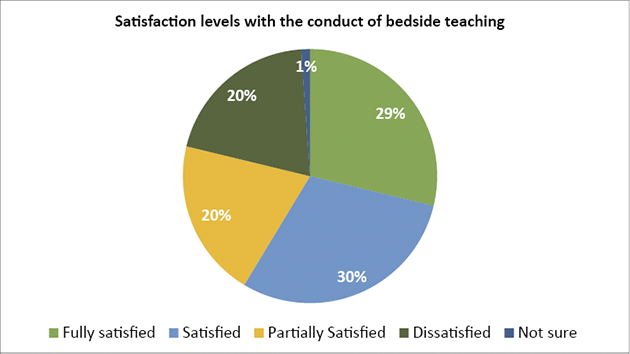
Figure 1. Satisfaction level of students with the conduct of bedside teaching
Discussion
Bedside teaching (BST) is an important and time-tested component of medical education [1, 2] to develop and enhance clinical and communication skills [3, 4] but, in recent years, various studies have documented a steady decline of BST [8, 9] resulting in a feeling of being unpreparedness among students when transitioning to clinical practice and this unpreparedness has been linked to the deterioration witnessed in the quality of clinical training at undergraduate course [10–11]. In this study, the students have pointed out the deficiency in the number and range of patients and outcomes of teaching related to certain topics like scrotum, trauma and anorectum appear worrisome. This is a concern that has been raised in many published studies from prestigious centres. Lawrentschuk and Bolton [14] conducted a study in 2003 enrolling 222 students in the final year of medical school at the University of Melbourne and found that 94% believed that Digital rectal examination (DRE) is an essential skill that they should learn before graduating, but only 52% felt they could give a confident opinion based on their DRE findings as the skill was taught improperly and the median number of DREs performed during training was only two, with 17% of students having never actually performed it even once. Only 24% had been made to feel a prostate cancer, 19% a rectal tumour, and 11% faecal constipation. The most often reason cited by the students for not performing DREs was the lack of a doctor to act as a supervisor. And hence, Lawrentschuk and Bolton [14] had concluded that a concerted effort was required from academics, supervising doctors and students to improve medical students’ proficiency in performing DRE. Turner and Brewster [15] in a study enrolling final-year medical students at Oxford Medical School, UK found that 44% had never felt a clinically malignant prostate gland and 41% weren’t at all confident’ in their ability to give an opinion based on their findings on a DRE. A recent study conducted by Beena and Jagadisan [16] also found a lack of importance given to DRE training of undergraduate students and huge gaps in imparting this otherwise very important clinical skill. However, in a study conducted by Eziyi et al. [17] at Ladoke Akintola University of Technology Teaching Hospital (LTH), Osogbo, Nigeria, 97.6% participating final year medical students agreed that they have been taught DRE and 80.3% have done one to five DRE. However, only in 38.6% of cases were the findings of the students on DRE always cross-checked by a trained faculty/doctor, as a result of which confidence levels were less.
In this study, 19 students (76%) had found the patients involved in bedside teaching had cooperated and displayed a positive attitude. This is highly encouraging. In a cross-sectional study conducted by Aljoudi et al. [18] at two university hospitals in Jeddah, Western Saudi Arabia, only 51% patients had displayed a positive attitude towards involving medical students in clinical examination and care. Female and young patients (<45 years old) were less likely to be comfortable and hence would have higher probability of displaying negative attitude. Patients have shown more willingness to get involved with medical students while taking history but were lesser comfortable with clinical examination.
Lesser availability of patients with clinical findings has been projected by the students in this study as a big drawback. This can be attributed partly to the development of day case surgery approach wherein there is admission of surgical patients to hospital for a planned surgical procedure, and discharge to home on the same day, without any chance of encounter with the medical students. Al-Swailmi et al. [19] in their qualitative study conducted at the Faculty of Medicine Northern Border University Arar, Kingdom of Saudi Arabia also identified non-availability of patients as a big barrier in bedside teaching and have suggested various measures including establishment of (i) free clinics for expatriates, and (ii) university hospital. The study also addressed the issue of patients’ co-operation and stressed upon the promotion of awareness among general public about students’ learning and its benefits. Simulation is an alternative to an actual patient and is effectively used to teach history taking, and examination techniques. Working with simulated patients or manikins before encountering real patients, tends to build good judgement and enhances the level of confidence since practicing with either can be repeated without any fear of annoying the patient [20].
In this study, at the end of the course, 21 students (84%) were either highly confident or else confident in communication skills. This is highly encouraging as BST has long been considered the most effective method to teach not only the clinical skills but also the communication skills and professionalism. Gat et al. [21] in 2016 described a novel model for BST, which emphasizes simultaneous clinical and communication teaching in a stepwise approach, and in their study the model was satisfactorily practiced by consecutive simulations with a gradual escalation of difficulty and adjusted instruction approaches.
In this study, 15 (60%) students were highly satisfied or else satisfied with the teaching faculty and 10 (40%) were either partially satisfied or else dissatisfied. Al-Swailmi et al. [19] had also found this factor in their study and stressed that proper faculty development programs have the potential to play a pivotal role in improving faculty skills and attitude. In the literature, there are various models that have been suggested to mitigate the faculty related adverse factors. Near-peer bedside clinical teaching wherein interns provide structured BST to final-year medical students as an adjunct to their formal teaching has been shown to be effective by Woods et al. [22] and Rashid et al. [23] in their respective studies. In the series by Rashid et al., 73.2% of final year students had stated that junior doctors delivered teaching that is comparable to that of consultant – led teaching and 97.9% had stated the revision course led by interns had a positive influence on their learning.
Limitations
The number of students enrolled in the study is less as this was a pilot project, but the results have still a potential to initiate positive changes in the actual conduct and execution of bedside teaching and later follow up with studies, to study the impact by using the very same questionnaire as a validated tool.
Conclusions and recommendations
Bedside teaching is a vital component of undergraduate medical education. Like elsewhere, there is a deficiency of suitable patients for bedside teaching. There is a need to mitigate the negative impact of this factor by various innovations like free clinics for expatriates and use of good quality mannequins and simulated patients. Faculty development sessions need to be organised for teachers to improve their teaching skills. After institution of corrective measures, a follow up study should be initiated to gauge the impact.
Acknowledgements. There is no source of funding nor any conflict of interest.
References
1. Peters M, Cate OT. Bedside teaching in medical education: a literature review. Perspect Med Educ 2014; 3(2): 76–88. DOI: 10.1007/s40037-013-0083-y.
2. Landry MA, Lafrenaye S, Roy MC, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics 2007; 120(2): 275–280. DOI: 10.1542/peds.2007-0107.
3. Kroenke K, Omori DM, Landry FJ, Lucey CR. Bedside teaching. South Med J 1997; 90(11): 1069–1074. DOI: 10.1097/00007611-199711000-00002.
4. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med 2008; 83(3): 257–264. DOI: 10.1097/ACM.0b013e3181637f3e.
5. Stone MJ. The wisdom of Sir William Osler. Am J Cardiol 1995; 75(4): 269–276. DOI: 10.1016/0002-9149(95)80034-p.
6. Murthy VK, Wright SM. Osler Centenary Papers: Would Sir William Osler be a role model for medical trainees and physicians today? Postgrad Med J 2019; 95(1130): 664–668. DOI: 10.1136/postgradmedj-2019-136646.
7. Aldeen AZ, Gisondi MA. Bedside teaching in the emergency department. Acad Emerg Med 2006; 13(8): 860–866. DOI: 10.1197/j.aem.2006.03.557.
8. Ahmed Mel-B K. What is happening to bedside clinical teaching? Med Educ 2002; 36(12): 1185–1188. DOI: 10.1046/j.1365-2923.2002.01372.x.
9. Garibaldi BT, Russell SW. Strategies to improve bedside clinical skills teaching. Chest 2021; 160(6): 2187–2195. DOI: 10.1016/j.chest.2021.06.055.
10. Burford B, Whittle V, Vance GHS. The relationship between medical student learning opportunities and preparedness for practice: a questionnaire study. BMC Med Educ 2014; 14(1): 223. DOI: 10.1186/1472-6920-14-223.
11. Monrouxe LV, Bullock A, Gormley G, Kaufhold K, Kelly N, Roberts CE, Mattick K, Rees C. New graduate doctors’ preparedness for practice: a multistakeholder, multicentre narrative study. BMJ Open 2018; 8(8): e023146. DOI: 10.1136/bmjopen-2018-023146.
12. Aljabarti A. Residents and teaching physicians’ perception about bedside teaching in non-clinical shift in the emergency department of King Abdul-Aziz Medical City, Jeddah, Saudi Arabia. Journal of Health Specialties 2018; 6(1): 1–13. DOI: 10.4103/jhs.JHS_6_17.
13. Serwah AA, Al Sulimani AA, Mohamed WS, Serwah MA, Alghamdy O, Almalky TS, Jawal AA. Assessment of the level of satisfaction of final year’s medical students with the clinical training at taif teaching hospitals, KSA. J Contemp Med Edu 2015; 3(2): 64–71. DOI: 10.5455/jcme.20150611063851.
14. Lawrentschuk N, Bolton DM. Experience and attitudes of final-year medical students to digital rectal examination. Med J Aust 2004; 181(6): 323–325. DOI: 10.5694/j.1326-5377.2004.tb06299.x.
15. Turner KJ, Brewster SF. Rectal examination and urethral catheterization by medical students and house officers: taught but not used. BJU Int 2000; 86(4): 422–426. DOI: 10.1046/j.1464-410x.2000.00859.x.
16. Beena A, Jagadisan B. Digital rectal examination training among Indian medical graduates. Clin Teach 2019; 16(1): 36–40. DOI: 10.1111/tct.12766.
17. Eziyi AK, Ademuyiwa AO, Eziyi JA, Salako AA. Digital rectal examination for prostate and rectal tumour: knowledge and experience of final year medical students. West Afr J Med 2009; 28(5): 318–322. DOI: 10.4314/wajm.v28i5.55011.
18. Aljoudi SB, Alsolami SS, Farahat FM, Alsaywid B, Abuznadah W. Patients’ attitudes towards the participation of medical students in clinical examination and care in Western Saudi Arabia. J Family Community Med 2016; 23(3): 172–178. DOI: 10.4103/2230-8229.189133.
19. Al-Swailmi FK, Khan IA, Mehmood Y, Al-Enazi SA, Alrowaili M, Al-Enazi MM. Students’ perspective of bedside teaching: a qualitative study. Pak J Med Sci 2016; 32(2): 351–355. DOI: 10.12669/pjms.322.9194.
20. Bokken L, Rethans JJ, Scherpbier AJ, van der Vleuten CP. Strengths and weaknesses of simulated and real patients in the teaching of skills to medical students: a review. Simul Healthc 2008; 3(3): 161–169. DOI: 10.1097/SIH.0b013e318182fc56.
21. Gat I, Pessach-Gelblum L, Givati G, Haim N, Paluch-Shimon S, Unterman A, Bar-Shavit Y, Grabler G, Sagi D, Achiron A, Ziv A. Innovative integrative bedside teaching model improves tutors’ self-assessments of teaching skills and attitudes. Med Educ Online 2016; 21: 30526. DOI: 10.3402/meo.v21.30526.
22. Woods R, Ramasubbu B, Donohoe C, Hennessy M. Near-peer bedside clinical teaching: example of a successful programme. Clin Teach 2014; 11(6): 472–477. DOI: 10.1111/tct.12195.
23. Rashid MS, Sobowale O, Gore D. A near-peer teaching program designed, developed and delivered exclusively by recent medical graduates for final year medical students sitting the final objective structured clinical examination (OSCE). BMC Med Educ 2011; 11: 11. DOI: 10.1186/1472-6920-11-11.