Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(1), pp. 34–39 DOI: https://doi.org/10.15388/LietChirur.2024.23(1).4
Transanal Hemorrhoidal Dearterialization (THD): A Single Center Experience on 100 Consecutive Cases
Aleksandar Mitevski
Faculty of Medical Sciences, Goce Delchev University, Stip, Macedonia
E-mail: aleksandar.mitevski@ugd.edu.mk
Vladko Cvetanovski
Faculty of Medical Sciences, Goce Delchev University, Stip, Macedonia
E-mail: vlatko.cvetanovski@ugd.edu.mk
Petar Markov
General Hospital Strumica, Macedonia
E-mail: petar.markov@ymail.com
Ilija Milev
Faculty of Medical Sciences, Goce Delchev University, Stip, Macedonia
E-mail: ilija.milev@ugd.edu.mk
Abstract. Introduction. Surgeons, using all available means for the treatment of the hemorrhoidal disease, must make compromises between the radicality of the potential surgical treatment (to prevent recurrence) and the maintenance of the postoperative functionality of the anorectum (avoiding stricture, anal fissures, incontinence, reduction of postoperative pain etc.). Materials and methods. All patients treated with the THD method using a system manufactured by THD S.p.A., Correggio, Italy, consisting of a proctoscope equipped with a Doppler probe and a light source was used to perform the operation. Results. Out of 100 operated patients, 64 (64%) were men and 36 (36%) were women. 54 patients had third degree hemorrhoidal disease, 32 had fourth degree, 7 patients had fourth degree hemorrhoidal disease with active bleeding and 7 patients had second degree hemorrhoidal disease with active bleeding. In the follow-up period, anal fissure formation in two patients and prolapse of a hemorrhoidal node in a treated patient with fourth-degree hemorrhoidal disease were noted. Discussion. It is estimated that more than 50% of the general population will experience at least one episode of symptomatic hemorrhoids during their lifetime. Morphological and hemodynamic changes that occur in patients with hemorrhoidal disease is the finding of an increased diameter of the terminal branches of the superior rectal artery that supplies the hemorrhoidal nodes. These branches are 10–11 in number, of which ligation of up to six is allowed for effective treatment with the THD method. Conclusion. If the THD technique is used according to the established standards, postoperative complications in patients in the form of fecal incontinence and chronic pain have not been described, which is also confirmed in our series. The absence of serious complications while addressing a hemorrhoidal disease at the level of the cause of its occurrence, makes the THD+mucopexy technique applicable in most cases. Correct manipulation of the instruments, precision in dearterization, mucopexy of the rectal mucosa and submucosa are imperative for achieving excellent results.
Keywords: hemorrhoids, dearterialization, mucopexy, transanal.
Received: 2023/11/30. Accepted: 2023/12/05.
Copyright © 2024 Aleksandar Mitevski, Vladko Cvetanovski, Petar Markov, Ilija Milev. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
In the search for methods for the treatment of hemorrhoidal disease from a historical point of view has led to a series of proposed therapeutic modalities that vary from dietary recommendations to radical surgery, depending on the degree of the disease and on the symptoms that the patient describes at the time of examination [1].
Painless discharge of bright blood is the most common manifestation of hemorrhoids. Perineal irritation or itching in the anus can be due to mucous secretion or fecal soiling in prolapsed hemorrhoids. A feeling of non-emptiness occurs in patients with larger hemorrhoidal nodes and the pain usually occurs when thrombosis occurs, almost always when an external hemorrhoid is involved, or when a fourth-degree internal hemorrhoid is strangulated.
Surgeons, using all available means for the treatment of the disease, must make compromises between the radicality of the potential surgical treatment (to prevent recurrence) and the maintenance of the postoperative functionality of the anorectum (avoiding stricture, anal fissures, incontinence, reduction of postoperative pain etc.). In order to reduce the complications associated with anorectal surgery, the development of treatment alternatives is aimed toward non-excisional techniques. In 1995 Morinaga et al. describe a new technique for the treatment of grade 2, 3, and 4 hemorrhoidal diseases by ligation of the hemorrhoidal arteries [2]. In 2007 Dal Monte et al. describe for the first time a modification of the THD/HAL procedure by introducing anopexy of prolapsed hemorrhoidal cushions [3].
In this paper we describe the results achieved in 100 consecutive cases of patients with 2, 3 and 4 degree hemorrhoidal disease treated with the THD+mucopexy method.
Materials and methods
All patients treated with the THD method are previously placed in a modified lithotomy position, under general anesthesia with a laryngeal mask in place. A system manufactured by THD S.p.A., Correggio, Italy consisting of a proctoscope equipped with a doppler probe and a light source was used to perform the operation. The probe uses a double crystal that allows more precise focusing of ultrasound waves and identification of larger diameter arteries located in the superficial layers of the rectal wall. The proctoscope itself has a sliding part that allows the distal direction of the continuous suture, during which the operator does not need to reposition the proctoroscope. The proctoscope is conical in shape with a rounded tip with an internal opening diameter ranging from 32–34 mm to 20–24 mm at the distal end. The suture used for the procedure is a 2–0 absorbable poglycol suture with a 5/8 needle.
The needle is placed on a specially designed needle holder with a marker on top for the level of its placement. By setting it at the marked level, the tip of the needle holder is inserted into the pivot of the proctoscope, which during the rotation of the needle ensures the standardization of the transfixation of the rectal mucosa with a maximum depth of up to 6.5 mm. This avoids fu ll-thickness rectal wall penetration and thus reduces the risk of perirectal fistula and abscesses. The THD kit also includes a knot pusher which can be useful in securing the initial suture as well as the mucopexy itself.
For easier performance of the procedure, cooperation with the anesthesiology team is required in the context of intraoperative blood pressure control, which should be maintained above 100–110 mmHg (systolic) in order to enable a better signal to the doppler when identifying the hemorrhoidal arteries.
Before the insertion of the proctoscope into the anal canal, it is necessary to lubricate it in order to maintain the situs and the length of the anal canal. Instrumental traction of the corresponding anal fold may be required in some cases. The insertion of the proctoscope ends when it reaches 6–7 cm from the anal verge. The starting position of the operation can be at any point on the rectal circumference and continue in any direction. With the placement of the proctoscope, the doppler is turned on, which aims to locate the 6 main stems of the hemorrhoidal arteries, which are usually located at 1, 3, 5, 7, 9 and 11 o’clock. Their exact location is determined by rotating the proctoscope and directing it towards the rectal wall. After obtaining a good pulsating signal, the proctoscope is pulled back following the artery distally, marking the level of the artery with the most pronounced pulsating signal. During this process, a variation is observed in the pulsating wave, which ranges from clearly present, through reduced or absent, to the most pronounced at the distal 2–3 cm of the rectum. It is due to the depth of the arteries in the rectal wall. At the proximal part the arteries can be located in the perirectal fatty tissue, at the level of reduction or absence the arteries perforate the rectal muscle and at the distal end where the arteries lie in the rectal submucosa.
After complete identification of the artery, the Doppler is turned off and the proctoscope is reinserted into the distal rectum. A “Z” suture is placed at the proximal fixation point. For this, the pivot of the rectoscope is used, in which the needle holder is rotated with the 5/8 needle in place. After the knot is tied, the proctoscope remains in place but its sliding part goes back, which exposes the rectal mucosa through which the suture passes every 5 mm and folds it along with the prolapsing submucosa longitudinally, up to the level of the placed marker where the last two stitches should be above and below the marker. Accomplishing that, the artery is sutured with the running suture and at that level dearterization is achieved. The mucopexy should stop at the beginning of the internal hemorrhoid cushion without its involvement. The operator should ensure that there is sufficient space between each of the vertical plication lines in order to avoid complete circumferential devascularization of the anus.
Results
Out of 100 operated patients, 64 (64%) were men and 36 (36%) were women. 54 patients had third degree hemorrhoidal disease, 32 had fourth degree, 7 patients had fourth degree hemorrhoidal disease with active bleeding and 7 patients had second degree hemorrhoidal disease with active bleeding.
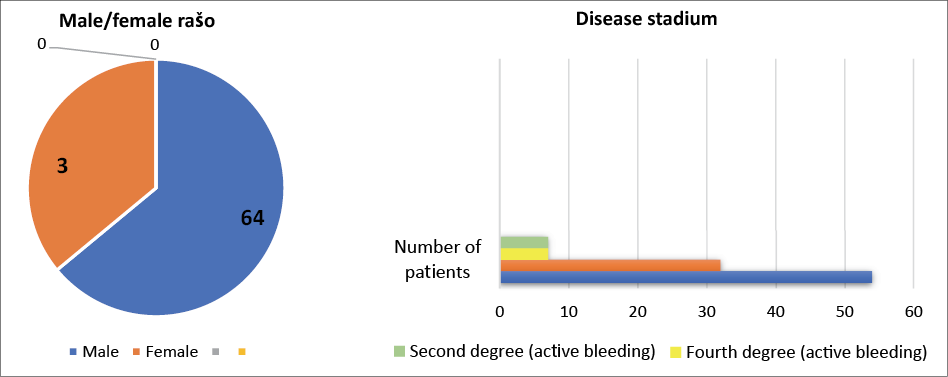
Figure 1. Patient distribution by sex and disease stadium
Table 1. Type and frequency of postoperative complications
|
Type of complication |
Anal fissure |
Prolapse of single |
Recurrence of the disease |
|
Number of patients |
2 |
2 |
3 total |
Patients presented with anamnestic data of occasional episodes of pain in the anal region, bleeding, daily need for repositioning of prolapsing hemorrhoidal nodes, daily discomfort and significantly affected daily functioning.
Data were recorded on the 1st and 7th postoperative and on 1st and 3th month after surgery. In the indicated follow-up period, anal fissure formation in two patients and a prolapse of a single fibrosed hemorrhoidal node in also two patients treated with fourth-degree hemorrhoidal disease were noted. Two recurrences were noted, one after 3 months, and 2 after two years.
Subjectively, a small number of patients complained of tightness, discomfort and mild pain in the anal region during the first three weeks of the operation.
Around 15 patients gave information of a feeling of prolapse during defecation and spontaneous reposition with no prolapse visible on examination or with straining. In these patients bleeding or any other symptoms were not present. On anoscopy reduced hemorroidal cushions were present without prolapsing.
|
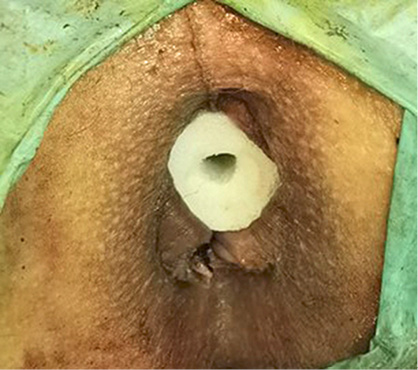
Figure 2. Patient before surgery |
Figure 3. Patient immediately after surgery |
|
Figure 4. Patient at first postoperative day |
Figure 5. Patient at 1 month follow up |
Discussion
Hemorrhoidal disease is one of the most frequent diseases in colorectal surgery for which a huge number of treatment methods have historically been proposed, some of which can be marked as controversial [4]. It is estimated that more than 50% of the general population will experience at least one episode of symptomatic hemorrhoids during their lifetime [5]. A plan for surgical treatment of symptomatic hemorrhoids is created and implemented only if conservative treatment methods have been exhausted and there is no improvement in symptomatology. Introducing a dietary regime and changing the lifestyle is a routine that is used in the treatment of hemorrhoidal disease in all stages of its progress, but also postoperatively to reduce complications and achieve the most desired effect of any surgical intervention. The purpose of these changes is to reduce straining during defecation, which is most often due to the inability to propel hard stool through the anal canal. Straining on the one hand, and, hard stools on the other, cause an increase in hemorrhoidal nodes and damage to the mucosa, which usually results in inflammation and bleeding in the later stages of the disease. It is the sliding anal canal theory that addresses the weakening of the supporting tissues of the anal pads, and hemorrhoids is actually the pathological term to describe this displacement causing venous dilatation [6].
Increasing water intake, changing the diet to high fiber products, supplementing them, and introducing stool softener oils or granules can reduce symptoms by up to 50% within 6 weeks of starting [7]. The above can be taken as a fact because theories about the formation of hemorrhoids as a result of varicose veins are slowly being rejected due to the fact that it is proven that varicose veins and hemorrhoids are different entities and in patients with portal hypertension and varicose veins there is no increased incidence of occurrence of hemorrhoids [8]. During the development of the hemorrhoidal disease, three main hemorrhoids located at 3, 7 and 11 o’clock appear mainly, with the possibility of the appearance of additional hemorrhoidal cushions between these three. The changes are the result of abnormal venous dilatation, vascular thrombosis and degenerative process of collagen fibers and fibroelastic tissues as well as distortion and rupture of the anal subepithelial muscle. All these changes are accompanied by an inflammatory reaction involving the vascular wall and surrounding connective tissue, with possible mucosal ulceration, ischemia and thrombosis [9].
Morphological and hemodynamic changes that occur in patients with hemorrhoidal disease is the finding of an increased diameter of the terminal branches of the superior rectal artery that supplies the hemorrhoidal nodes. These branches are 10–11 in number, of which ligation of up to six is allowed for effective treatment with the THD method. Also, in these patients, increased blood flow, higher terminal flow velocity and higher flow acceleration are noted compared to findings in healthy subjects [10]. The theory of the occurrence of hemorrhoids as a result of abnormal venous dilatation and disturbed regulation of vascular tone is based on histological findings obtained after histological examination of removed hemorrhoidal nodes. Vascular smooth muscle is regulated by the autonomic nervous system, hormones, cytokines, and the endothelium. A disproportion between endothelium-derived relaxing factors and its vasoconstrictor factors causes such disorders [11]. Disturbances in the anal region contribute to an increase in anal pressure, reduced rectal compliance and greater perineal descent, an effect that disappears 3–4 months after surgical treatment [12].
Conclusion
If the THD technique is used according to the established standards, postoperative complications in patients in the form of fecal incontinence and chronic pain have not been described, which is also confirmed in our series. The absence of serious complications and the addressing of hemorrhoidal disease at the level of the cause of its occurrence, makes the THD+mucopexy technique applicable in most cases. Correct manipulation of the instruments, precision in dearterization, mucopexy of the rectal mucosa and submucosa are imperative for achieving excellent results. An important segment in the postoperative course is the discipline of the patients to adhere to the hygiene and dietary recommendations at least in the first month after the procedure.
References
1. Kaidar-Person O, Person B, Wexner SD. Hemorrhoidal disease: A comprehensive review. J Am Coll Surg 2007; 204(1): 102–117.
2. Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol 1995; 90(4): 610–613.
3. Dal Monte PP, Tagariello C, Sarago M, Giordano P, Shafi A, Cudazzo E, Franzini M. Transanal haemorrhoidal dearterialisation: nonexcisional surgery for the treatment of haemorrhoidal disease. Tech Coloproctol 2007; 11(4): 333–338; discussion 338–339.
4. Pata F, Gallo G, Pellino G, Vigorita V, Podda M, Di Saverio S, D’Ambrosio G, Sammarco G. Evolution of surgical management of hemorrhoidal disease: An historical overview. Front Surg 2021; 8: 727059. DOI: 10.3389/fsurg.2021.727059.
5. The Standards Task Force American Society of Colon and Rectal Surgeons. Practice parameters for the treatment of hemorrhoids. Dis Colon Rectum 1990; 33(11): 992–993. DOI: 10.1007/BF02139115.
6. Thomson WH. The nature of haemorrhoids. Br J Surg 1975; 62(7): 542–552.
7. Moesgaard F, Nielsen ML, Hansen JB, Knudsen JT. High–fiber diet reduces bleeding and pain in patients with hemorrhoids: a double–blind trial of Vi–Siblin. Dis Colon Rectum 1982; 25(5): 454–456.
8. Goenka MK, Kochhar R, Nagi B, Mehta SK. Rectosigmoid varices and other mucosal changes in patients with portal hypertension. Am J Gastroenterol 1991; 86(9): 1185–1189.
9. Morgado PJ, Suárez JA, Gómez LG, Morgado PJ Jr. Histoclinical basis for a new classification of hemorrhoidal disease. Dis Colon Rectum 1988; 31(6): 474–480.
10. Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R, Fritsch H. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis 2009; 24(1): 105–113.
11. Stankevicius E, Kevelaitis E, Vainorius E, Simonsen U. [Role of nitric oxide and other endothelium–derived factors.] Medicina (Kaunas) 2003; 39(4): 333–341.
12. Ho YH, Seow-Choen F, Goh HS. Haemorrhoidectomy and disordered rectal and anal physiology in patients with prolapsed haemorrhoids. Br J Surg 1995; 82(5): 596–598.