Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(1), pp. 45–51 DOI: https://doi.org/10.15388/LietChirur.2024.23(1).6
Iatrogenic Tracheal Rupture after Endotracheal Intubation: A Case Report
Silvana Kraleva
Department of Anesthesiology and Intensive Care, City General Hospital “8th September”, Skopje, North Macedonia
E-mail: silvanakraleva@yahoo.com
Tatjana Trojikj
Department of Anesthesiology and Intensive Care, City General Hospital “8th September”, Skopje, North Macedonia
Faculty of Medical Sciences, Goce Delchev University, Stip, North Macedonia
E-mail: tanja.trojik@gmail.com
Darko Talevski
Department of Orthopedic Surgery ant Traumathology, City General Hospital “8th September”, Skopje, North Macedonia
E-mail: darko_talevski@yahoo.com
Dola Malefski
Department of Anesthesiology and Intensive Care, City General Hospital “8th September”, Skopje, North Macedonia
E-mail: Dolashkembi@yahoo.com
Gordana Bozinovska Beaka
Department of Abdominal Surgery, City General Hospital “8th September”, Skopje, North Macedonia
Faculty of Medical Sciences, Goce Delchev University, Stip, North Macedonia
E-mail: g.bozinovska.beaka@gmail.com
Abstract. Iatrogenic tracheal rupture is very rare condition and has a lot off causes (intubation, tracheostomy, bronchoscopy, esophagectomy), but orotracheal intubation is the most common. Diagnosis is based on the occurrence of symptoms that are not specific but highly suggestive: subcutaneous emphysema, respiratory insufficiency, pneumothorax, and hemoptysis. The appearance of subcutaneous emphysema as a first sign plays a main role for early diagnosis and rapid appropriate treatment. Diagnostic confirmation is possible by chest X-ray, thoracic computed tomography and bronchoscopy which confirmed the size and site of the lesion. Treatment can be conservative, in patients with small ruptures, less than 2 cm, and surgical in the majority of ruptures over 2 cm in length.
Our case report presents an iatrogenic post-intubation tracheal rupture treated conservatively. Our patient was a 71-year-old woman, admitted in our hospital with fracture of right humerus for elective surgery. Her medical history was only arterial hypertension. She underwent general anesthesia, intubated with flexible ET tube, positioned in beach-chair position after introduction, and no complication occurred during surgery. 18 hours after surgery, after severe coughing, she suddenly developed subcutaneous emphysema of the facial, neck and upper anterior chest. Tracheal rupture was confirmed with a thoracic computed tomography and tracheobronchial fiber endoscopy. It showed a posterior tracheal transmural rupture 1 cm long, located 4 cm above the carina, covered with small tissue that opened in inspirium. Conservative treatment with antibiotic cover was performed, and the patient was discharged home in good condition, fourteen days after the initial injury.
Keywords: tracheal rupture, endotracheal intubation, subcutaneous emphysema, pneumothorax, computed tomography, tracheobronchial fiber endoscopy, conservative treatment, surgical treatment.
Received: 2023/09/25. Accepted: 2023/10/26.
Copyright © 2024 Silvana Kraleva, Tatjana Trojikj, Darko Talevski, Dola Malefski, Gordana Bozinovska Beaka. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Iatrogenic tracheal rupture is very rare condition and has a many causes (intubation, tracheostomy, bronchoscopy, placement of stents, esophagectomy, and others), though orotracheal intubation is the most common [1]. This injury is associated with a high percentage of morbidity and mortality. Diagnosis is based on the occurrence of symptoms that are not specific but highly suggestive: subcutaneous emphysema, respiratory insufficiency, pneumothorax, and hemoptysis. Diagnostic confirmation is possible by chest X-ray, thoracic computed tomography and bronchoscopy, which will confirm the size and site of the lesion. The treatment of choice has been urgent surgical repair, although the authors of the largest series now preferred conservative treatment whenever permitted by the lesion and state of the patient. However, the group of patients who would benefit from surgical treatment has not been fully defined [2].
The most common clinical signs of iatrogenic tracheal rupture are subcutaneous and mediastinal emphysema, and pneumothorax. Other signs can be dyspnea, dysphonia, cough, hemoptysis, and pneumoperitoneum [3]. These signs can appear immediately after extubation, or they can take a few hours or days to appear. It is interesting to know that the appearance of subcutaneous emphysema is not only the most common symptom, it is a protective factor, as reflected in the findings of the meta-analysis of Wagner et al. [4], and its presence warns to the possible tracheal rupture, starting the procedures for its diagnosis and correct treatment.
After clinical suspicion, diagnostic confirmation must be done, which is possible by direct visualization by bronchoscopy. This procedure gives us the exact position and extension of the rupture, helps us to plan the type of therapeutic treatment, and can be useful for reposition the tube or reintubate the patient if it is necessary [3]. Tracheal ruptures are usually longitudinal and are most frequently located in the pars membranosa, the posterior part of the trachea that lacks cartilaginous support [5]. Prolonged diagnosis leads to the onset of mediastinitis, with deterioration in the clinical situation [6].
Until now, there is still no common consensus on the management of iatrogenic tracheal rupture after intubation. Early surgical treatment has traditionally been the choice of treatment [7]. It is justified by offering good results and that the prognosis will generally depend on the presenting disease rather than on the tracheal damage itself [8]. However, a lot of authors prefer conservative treatment in patients with small ruptures, less than 2 cm, and in selected patients with minimal, non-progressive symptoms and with no air leakage on spontaneous breathing [9–11]. If the ruptures are longer than 2 cm, there are big differences of opinion. Some authors preferred surgical treatment in the majority of ruptures over 2 cm in length [6], while other authors recommend surgery only in those ruptures caused by intubation prior to thoracic surgery and in ruptures that give rise to immediate symptoms. However, authors of more recent publications propose conservative management to be the treatment of choice [12]. Patients who are clinically stable, on spontaneous breathing, with no respiratory difficulty or air leakage, no esophageal damage, minimal mediastinal collections, no signs of clinical progression (emphysema or pneumomediastinum), and no symptoms of infection, and patients in whom extubation is likely to occur within the following 24 hours or who require mechanical ventilation to treat an underlying respiratory problem, should be managed conservatively [10]. This treatment includes intubation, the cuff should be positioned distal to the area of rupture, continuous tracheal aspiration, a pleural drain if needed, and antibiotic therapy [13]. The choices for surgical treatment are multiple and will depend on the type and size of the lesion. Minimally invasive techniques, such as video thoracoscopy can be used [14].
In summary, although post-intubating tracheal rupture is a rare condition, it is associated with high morbidity and mortality. Clinical suspicion is essential, with fast confirmation by bronchoscopy. This entity is most common in elderly women, although the risk of death is higher in men. The risk factor that leads to increase in the risk of death is emergency intubation in comparison with elective intubation. Subcutaneous emphysema is a protective factor that leads to early diagnosis and treatment. Conservative treatment is associated with a better outcome, but it is not clear which group of patients will benefit from surgical treatment. And, greater training of the staff who manage the airway could reduce the incidence of iatrogenic tracheal rupture.
Case report
Our patient was a 71-year-old woman, admitted in the hospital with fracture of right humerus. Her body weight was 61 kg, body height around 160 cm. Her only medical history was arterial hypertension that was treated with lisinopril 10 mg/day and bisoprolol 2,5 mg/day. She didn’t smoke and had no history of COPD, but preoperative chest X-ray showed designated pulmonary pattern and interstitium with peripheral hyperinflation, designated hilusses with coarse confluent shadows infrahilary. Rivaroxaban because of fracture was stopped 3 days ago.
She underwent general anesthesia for the surgery. No complication occurred during and immediately after surgery. She was intubated with single lumen flexible tube number 7, with stylet in, and oral intubation was performed without difficulty, at first attempt. After introduction, our patient was positioned in beach-chair position. The surgery lasted approximately 90 minutes. Extubation was done in the operation room and patient with stable vital signs was sent to the ward.
Next morning, 18 hours after surgery the anesthesiologist was requested because the patient, after severe coughing, had suddenly developed subcutaneous emphysema of the facial, bilateral latero-cervical and upper anterior chest. She was scared, but not dyspneic, with normal bilateral breathing on auscultation and stable vital signs, SpO2 = 97–98% without oxygen therapy.
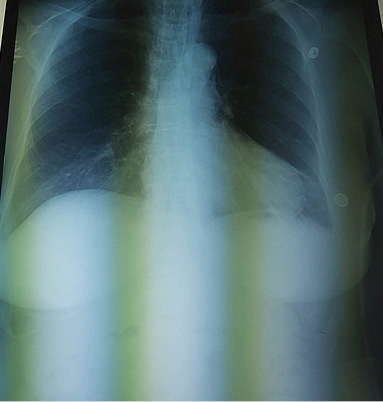
The chest X-ray was done immediately and did not present any abnormal signs, only small subcutaneous emphysema in the neck (Figure 1).
|
|
|
|
Figure 1. Chest X-ray |
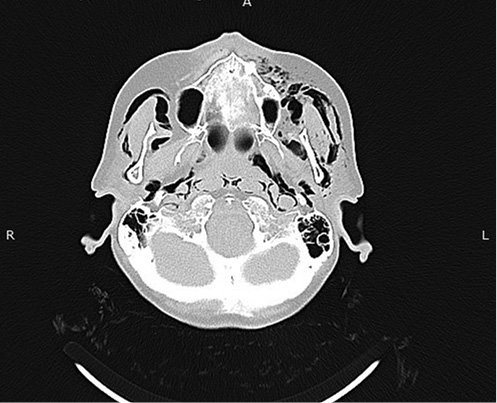
Figure 2. Diffuse soft tissues emphysema |
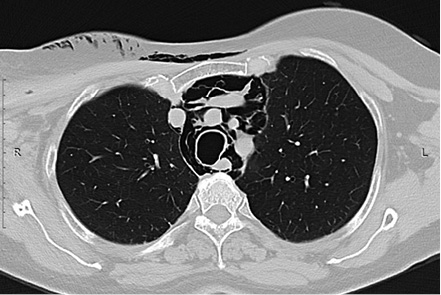
A cranial and thoracic computed tomography (CT) showed diffuse soft tissues emphysema from the thoracic region to the neck and face (Figure 2), and mediastinal emphysema in all compartments (Figure 3), and interruption of tracheal continuity 4 cm cranial from the bifurcation (Figure 4).
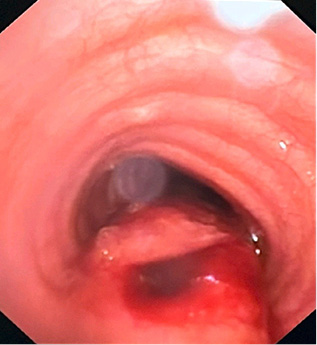
No pneumothorax was observed. Traumatic tracheal rupture was suspected, and emergency tracheobronchial fiber endoscopy confirmed the diagnosis. It showed a posterior tracheal transmural rupture 1 cm long, located 4 cm above the carina, covered with small tissue that opened in inspirium (Figure 5). The patient was admitted in the Intensive Care Unit, oxygen therapy started, and vital signs were monitored.
|
Figure 3. Mediastinal emphysema |
Figure 4. Interruption of tracheal continuity |
|
|
|
Thoracic surgeon opinion was that the location of the lesion and its size favoured conservative treatment with antibiotic cover (meropenem and metronidazole) and monitoring in the Intensive Care Unit. The patient improved, and five days later, the chest X-ray showed markedly less mediastinal and subcutaneous emphysema. She was sent to the surgical ward, and after seven more days, the patient was discharged home in good condition, fourteen days after the initial injury.
Discussion
Orotracheal intubation is a routine procedure performed every day, but has potential complications. Despite the large number of intubations, these complications are rare. They include throat pain, laryngitis, glottic edema, mucosal ulceration, laryngeal or tracheal stenosis, necrosis of the tracheal wall, fistulas, aspiration, esophageal intubation, bronchial intubation, atelectasis, and tracheal rupture [15]. Tracheal disruption after intubation is a rare entity [16]. Because of that, we do not have adequate prospective studies to evaluate its incidence. Despite these limitations, it was estimated that the incidence of tracheal rupture after intubation is of 1/20 000 intubations, and it varies depending on the publication [17].
The exact mechanism of this injury is unknown. There are a lot of risk factors for tracheal rupture after intubation and can be divided into mechanical and anatomical. Mechanical factors include multiple attempts at intubation, inexperience of the doctors that performed intubation, endotracheal tube introducers that protrude beyond the tip of the tube, overinflated cuff (diffusion of nitric oxide into the cuff), incorrect position of the tip of the tube, repositioning the tube without deflation of the cuff, bigger size of the tube, significant cough after intubation, and movements of the head and neck while the patient is intubated [13]. The anatomical factors include congenital tracheal abnormalities, weakness of the pars membranosa of the trachea, chronic obstructive pulmonary disease and other inflammatory lesions of the tracheobronchial tree, diseases that alter the position of the trachea (mediastinal collections, lymph nodes, or tumors), chronic use of steroids, advanced age, and female sex [4]. The study by Chen et al. [18], who performed a literature review, defined an at-risk population that included women over 50 years of age who required intubation with double-lumen tubes and/or excessive pressure of the tube cuff.
Some authors have suggested that post intubation tracheal rupture may be presented more frequently in women because the pars membranosa is weaker in women than in men [4], due to the use of endotracheal tubes of a larger size than appropriate for women, or that women are not as tall and, therefore, the endotracheal tube is positioned significantly more distantly in a trachea that is already smaller [19]. The incidence of female patients with iatrogenic tracheal rupture has been previously observed and correlation has led to the conclusion that a membranous trachea is less firm in women than in men, but this could be due to the use of an oversized tube rather than for constitutional reasons. Other authors have suggested that a short stature could be a predisposing factor for this lesion; in the studies by Marty-Ané et al. [13] and by Massard et al. [20] all the patients had a height under 165 cm. Hoffman et al. [21] also reported that 50% of their patients had a height under 160 cm. Often, this complication can be caused by a combination of these factors, but in some of the cases, the cause is unknown.
Our patient was at-risk population that includes women over 50 years of age, she was not as tall (160 cm), she was intubated with ET tube with stylet in, and after that sited in beach-chair position. Cuff pressure we couldn’t measure. Some interesting information from our patient she gave us is that, her profession was a teacher, and she was working a lot using chalk to write on the school blackboard.
As we mentioned, the most common clinical manifestations of post intubating tracheal rupture are subcutaneous emphysema, mediastinal emphysema, and pneumothorax. These signs often develop immediately or soon after extubation, although they can take several hours or days to appear. In our case, subcutaneous emphysema as a first sign was manifested 16 hours after extubation, and it had protective role because it alarmed us to start with diagnostic procedures. Chest X-ray and chest and cranial CT scan were done immediately and showed soft tissues emphysema, pneumomediastinum, but for confirming the tracheal rupture, position, and size, tracheobronchial fiber endoscopy was done. It helped us approximately to determine the type and extension of the rupture and right decision for treatment.
An adequate therapeutic strategy of a post-intubation tracheal rupture is dependent on the size and the location of the rupture, its clinical manifestation, and the condition of the patient. Two therapeutic strategies are in option: conservative and surgical treatment. Which is the best treatment for tracheal rupture after tracheal intubation is challenging. The tendency is to decrease invasive surgical treatment for the benefit of conservative management. Surgical repair is the preferred treatment for those patients when a transmural lesion with a length above 2 cm causes pneumothorax and/or pneumomediastinum and when the lesion is discovered during a thoracic surgical procedure [22]. Conservative treatment may be a viable alternative for some patients [23]. The conservative treatment can include mechanical ventilation after tracheal or bilateral endobronchial intubation with the cuff inflated distal to the lesion, chest drain, broad-spectrum antibiotics (using a combination of beta-lactam and aminoglycoside because mediastinitis and sepsis can occur in the long term), and chest physiotherapy.
Selection of treatment for post-intubation tracheal rupture must be individualized. But some cases illustrate the current tendency to increase conservative therapy in this pathology [24].
In our case, we started with conservative therapeutical treatment because of small rupture, less than 2 cm, minimal non-progressive symptoms and no air leakage on spontaneous breathing. At the end, the patient made a full and uncomplicated recovery and was discharged fourteen days after the original injury. This case report presented the non-surgical therapeutic strategy of a post-intubating tracheal injury.
Conclusion
In summary, tracheal iatrogenic rupture after endotracheal intubation is a rare condition but associated with high morbidity and mortality, most common in elderly women, although the risk of death is higher in men. The appearance of subcutaneous emphysema is a protective factor as it alarms us for early diagnosis and the rapid initiation of the appropriate treatment. Treatment can be conservative, associated with a better outcome, or surgical treatment.
Our case report presented an iatrogenic post-intubation tracheal rupture treated conservatively. And we can conclude that greater training of the staff, especially anesthesiologists could reduce the incidence of iatrogenic tracheal rupture.
References
1. Berry M, Van Schil P, Van Meerbeeck J, Vanmaele R, Eyskens E. Surgical treatment of iatrogenic tracheal lacerations. Acta Chir Belg 1997; 97(6): 308–310.
2. Miñambres E, Burón J, Ballesteros MÁ, Llorca J, Muñoz P, González-Castro A. Tracheal rupture after endotracheal intubation: a literature systematic review. Eur J Cardiothorac Surg 2009; 35(6): 1056–1062.
3. Hasan A, Low DE, Ganado AL, Norton R, Watson DCT. Tracheal rupture with disposable polyvinylchloride double-lumen endotracheal tubes. J Cardiothorac Vasc Anesth 1992; 6(2): 208–211.
4. Wagner A, Roeggla M, Hirschl MM, Roeggla G, Schreiber W, Sterz F. Tracheal rupture after emergency intubation during cardiopulmonary resuscitation. Resuscitation 1995; 30(3): 263–266.
5. Lobato EB, Risley 3rd WP, Stoltzfus DP. Intraoperative management of distal tracheal rupture with selective bronchial intubation. J Clin Anesth 1997; 9(2): 155–158.
6. Sippel M, Putensen C, Hirner A, Wolff M. Tracheal rupture after endotracheal intubation: experience with management in 13 cases. Thorac Cardiovasc Surg 2006; 54(1): 51–56.
7. Mussi A, Ambrogi MC, Menconi G, Ribechini A, Angeletti CA. Surgical approaches to membranous tracheal wall lacerations. J Thorac Cardiovasc Surg 2000; 120(1): 115–118.
8. Kumar SM, Pandit SK, Cohen PJ. Tracheal laceration associated with endotracheal anesthesia. Anesthesiology 1977; 47(3): 298–299.
9. d’Odemont JP, Pringot J, Goncette L, Goenen M, Rodenstein DO. Spontaneous favorable outcome of tracheal laceration. Chest 1991; 99(5): 1290–1292.
10. Conti M, Pougeoise M, Wurtz A, Porte H, Fourrier F, Ramon P, Marquette CH. Management of postintubation tracheobronchial ruptures. Chest 2006; 130(2): 412–418.
11. Gómez-Caro Andrés A, Moradiellos Díez FJ, Ausín Herrero P, Díaz-Hellín Gude V, Larrú Cabrero E, de Miguel Porch E, Martín De Nicolás JL. Successful conservative management in iatrogenic tracheobronchial injury. Ann Thorac Surg 2005; 79(6): 1872–1878.
12. Jougon J, Ballester M, Choukroun E, Dubrez J, Reboul G, Velly JF. Conservative treatment for postintubation tracheobronchial rupture. Ann Thorac Surg 2000; 69(1): 216–220.
13. Marty-Ané CH, Picard E, Jonquet O, Mary H. Membranous tracheal rupture after endotracheal intubation. Ann Thorac Surg 1995; 60(5): 1367–1371.
14. Törnvall SS, Jackson KH, Oyanedel E. Tracheal rupture, complication of cuffed endotracheal tube. Chest 1971; 59(2): 237–239.
15. Thompson DS, Read RC. Rupture of the trachea following endotracheal intubation. JAMA 1968; 204(11): 995–997.
16. Carbognani P, Bobbio A, Cattelani L, Internullo E, Caporale D, Rusca M. Management of postintubation membranous tracheal rupture. Ann Thorac Surg 2004; 77(2): 406–409.
17. Orta DA, Cousar 3rd JE, Yergin BM, Olsen GN. Tracheal laceration with massive subcutaneous emphysema: a rare complication of endotracheal intubation. Thorax 1979; 34(5): 665–669.
18. Chen EH, Logman ZM, Glass PS, Bilfinger TV. A case of tracheal injury after emergent endotracheal intubation: a review of the literature and causalities. Anesth Analg 2001; 93(5): 1270–1271.
19. Kaloud H, Smolle-Juettner FM, Prause G, List WF. Iatrogenic ruptures of the tracheobronchial tree. Chest 1997; 112(3): 774–778.
20. Massard G, Rougé C, Dabbagh A, Kessler R, Hentz JG, Roeslin N, Wihlm JM, Morand G. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg 1996; 61(5): 1483–1487.
21. Hofmann HS, Rettig G, Radke J, Neef H, Silber RE. Iatrogenic ruptures of the tracheobronchial tree. Eur J Cardiothorac Surg 2002; 21(4): 649–652.
22. Gabor S, Renner H, Pinter H, Sankin O, Maier A, Tomaselli F, Smolle Jüttner FM. Indications for surgery in tracheobronchial ruptures. Eur J Cardiothorac Surg 2001; 20(2): 399–404.
23. Beiderlinden M, Adamzik M, Peters J. Conservative treatment of tracheal injuries. Anesth Analg 2005; 100(1): 210–214.
24. Prunet B, Lacroix G, Asencio Y, Cathelinaud O, Avaro JP, Goutorbe P. Iatrogenic post–intubation tracheal rupture treated conservatively without intubation: a case report. Cases J 2008; 1(1): 259. DOI: 10.1186/1757-1626-1-259.