Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(2), pp. 113–119 DOI: https://doi.org/10.15388/LietChirur.2025.24(2).4
Multiple Recurrent Bilateral Ovarian Teratomas: A Case Report and Comprehensive Review
Aušrinė Anužytė
Vilniaus universitetas, Medicinos fakultetas, Vilnius, Lietuva
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
E-mail: ausrineanu@gmail.com
https://ror.org/03nadee84
Eglė Noreikaitė
Vilniaus universitetas, Medicinos fakultetas, Vilnius, Lietuva
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
E-mail: egle.noreikaite@gmail.com
https://ror.org/03nadee84
Viktorija Žitkutė
Vilniaus universitetas, Medicinos fakultetas, Vilnius, Lietuva
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
Akušerijos ir ginekologijos centras, Vilniaus universiteto ligoninė Santaros klinikos, Vilnius, Lietuva
Center of Obstetrics and Gynaecology, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: viktorijazitkute@gmail.com
https://ror.org/03nadee84
Linas Andreika
Vilniaus universitetas, Medicinos fakultetas, Vilnius, Lietuva
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
Akušerijos ir ginekologijos centras, Vilniaus universiteto ligoninė Santaros klinikos, Vilnius, Lietuva
Center of Obstetrics and Gynaecology, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: linas.andreika@santa.lt
https://ror.org/03nadee84
Abstract. Background. Dermoid ovarian cyst or mature cystic teratoma is the most common subtype of ovarian germ cell tumors. These tumors are usually benign and contain hair, bone, primitive or mature teeth, cartilage, nerve and fat. The aim of this article is to present a case of multiple recurrent bilateral ovarian teratomas and to review literature on this topic. Case presentation. We present the case of a 25-year-old woman complaining of pain in the left abdomen, persisting for a year. All laboratory tests were within normal range, aside from elevated testosterone level. Intrauterine ultrasound and pelvic MRI revealed multiple dermoid cysts varying in size bilaterally. Laparoscopic ovarian cystectomy was performed and teratomas containing hair and fat were removed. During follow-up checkups a new 1 cm hyperechogenic mass, possibly a recurrent dermoid cyst, was observed in the right ovary. Conclusions. Ovarian dermoid cysts are a common benign ovarian tumor, usually found incidentally. They are often asymptomatic, occasionally presenting with abdominal pain or hormonal effects. The treatment strategy depends on many factors, but large, symptomatic cysts often require surgical management. Ovarian teratomas have a small chance of recurrence.
Keywords: dermoid ovarian cyst, mature cystic teratoma, laparoscopic ovarian cystectomy.
Daugybinės pasikartojančios abipusės kiaušidžių dermoidinės cistos: klinikinis atvejis ir literatūros apžvalga
Santrauka. Įvadas. Dermoidinė kiaušidžių cista, arba brandi cistinė teratoma, – labiausiai paplitęs kiaušidžių germinacinių ląstelių navikų potipis. Dažniausiai šie navikai, kurių sudėtyje randama plaukų, kaulų, dantų, kremzlių, nervų ir riebalų, yra gerybiniai. Straipsnio tikslas – pristatyti daugybinių pasikartojančių abipusių kiaušidžių teratomų atvejį ir apžvelgti mokslinę literatūrą šia tema. Klinikinis atvejis. Pristatomas 25 m. moters, kuri metus laiko kentėjo skausmą kairėje apatinėje pilvo pusėje, klinikinis atvejis. Pacientei nustatytas padidėjęs testosterono kiekis, kiti laboratoriniai tyrimai buvo nepakitę. Atlikus ultragarsinį tyrimą transvaginaliai ir dubens MRT, abiejose kiaušidėse pastebėta daugybinių brandžių cistinių teratomų. Laparoskopinės kiaušidžių cistektomijos metu pašalintos teratomos, turėjusios plaukų ir riebalų. Vėliau atliekant patikrą dešinėje kiaušidėje rasta nauja 1 cm hiperechogeninė masė, galimai dermoidinė cista.
Išvados. Kiaušidžių dermoidinė cista – dažnas gerybinis kiaušidžių navikas, dažniausiai randamas atsitiktinai. Šioms cistoms būdinga simptomatika – apatinės pilvo dalies skausmas. Retais atvejais galimi hormonų sutrikimai. Gydymo strategija priklauso nuo daugelio veiksnių, tačiau, nustačius didelę simptominę cistą, įprastai taikomas chirurginis gydymas. Yra nedidelė tikimybė, kad kiaušidžių teratomos gali kartotis.
Reikšminiai žodžiai: dermoidinė kiaušidžių cista, brandi cistinė teratoma, laparoskopinė kiaušidės cistektomija.
Received: 2025 03 18. Accepted: 2025 04 10.
Copyright © 2025 Aušrinė Anužytė, Eglė Noreikaitė, Viktorija Žitkutė, Linas Andreika. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Dermoid ovarian cysts or mature cystic teratomas are benign, well-differentiated germ cell tumors with all three layers: endoderm, ectoderm, and mesoderm [1, 2]. Dermoid ovarian cysts are often associated with findings of hair, immature or mature teeth, nerves, bones, cartilage, and subaccount materials in their structure. They are classified as benign mature (well-differentiated), malignant immature or monodermal teratomas [3]. Dermoid ovarian cysts are the most common subtype of ovarian germ cell tumors, which make up 11–15% of all ovarian tumors, 69% of all germ cell tumors, and 90–95% of teratomas [3]. Dermoid cysts occur more on the right ovary [4]. Dermoid ovarian cysts are bilateral in 10–15% of the cases [5], and around 4% of cases tend to recur [6]. Based on the literature review, these cysts can occur in any age group [7], but the incidence rate is highest among women of reproductive age (15–40 years) [4, 8]. Multiple theories are used to explain the origin of teratomas. Firstly, a blastomere theory was suggested; this theory explains that teratomas arise from residual pluripotential embryonic cells that are left behind after a missed abortion or an unborn fetus papyraceous [9]. However, this hypothesis has been disproved as teratoma cells have a 46, XX karyotype, meaning they can only come from the host and have completed meiosis. This is where the imperfect parthenogenesis theory comes from. The latter is the most popular theory so far. Linder et al. [10] suggested that dermoid ovarian cyst arises from self-fertilization cells after the first meiotic division by the failure of meiosis II. This particular theory could also be used to explain that there may be a genetic defect responsible for inciting parthenogenesis, and it can be transmitted from one generation to the next [11]. Lastly, primordial germ cell (PGC) theory postulates that PGCs develop among the yolk sac’s endodermal cells near the allantois’s origin and migrate to the gonadal ridges. Some cells, however, get displaced and can result in a teratoma anywhere in the human body, including the brain, stomach, and the sacrococcygeal region [12, 13].
Case presentation
A 25-year-old nulliparous woman with regular menstrual periods consulted a gynecologist because of pain in the left lower abdomen, especially when inserting a menstrual cup or tampon. This pain had persisted for a year. She had no vaginal discharge, fever, dysuria, frequent urination, or diarrhea. Additionally, this woman was consulted by an endocrinologist and a dermatologist for hair loss. Testosterone level was elevated, and she was taking spironolactone for six months. CA125 level and other laboratory values were normal. Transvaginal ultrasound showed larger bilateral ovaries, left ovary enlarged to 4.5x2.5 cm with multiple cysts 2–3 cm in size with echo positive inserts, and right ovary also enlarged to 6.9x4.0 cm with cyst 4.0x3.8 cm in size filled with opaque content (Figure 1, 2).
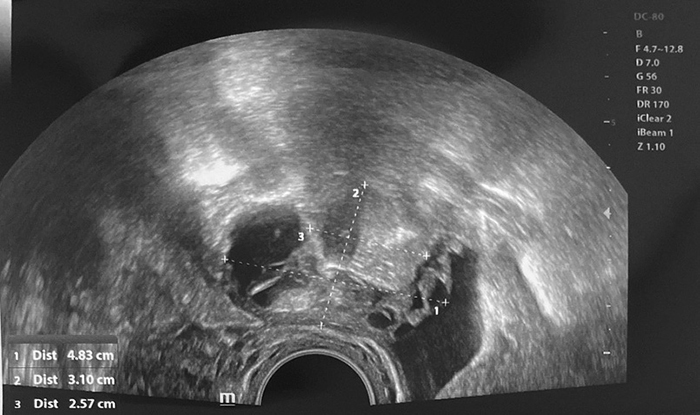
Figure 1. Right ovary
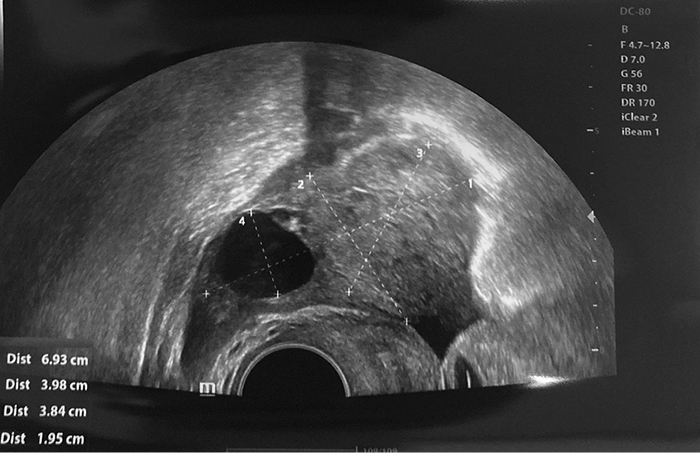
Figure 2. Left ovary
A pelvic MRI showed three dermoid cysts on the right ovary, the largest of which was 3.2 cm. The left ovary also showed five dermoid cysts, the largest 4.2 cm diameter. A bilateral laparoscopic ovarian cystectomy was performed. During the operation, dermoid cysts containing hair and fat were found in both ovaries. With the help of bipolar coagulator and forceps, three right ovarian dermoid cysts and five left ovarian dermoid cysts were enucleated. To preserve the largest possible ovarian reserve, the ovaries were minimally coagulated and sutured to ensure hemostasis. Histopathological findings confirmed mature benign teratomas on both sides with no immature tissue. These non-malignant tumors had multi-layered squamous epithelium, mature adipose, and nervous tissue with inclusions of keratin masses. After 6 and 12 months, the patient came for a follow-up checkup. At both time points, ultrasound showed that the bilateral ovaries were normal in size with sufficient reserve (the antral follicle count was 6 to 8 in both ovaries). Still, a minor about 10 mm hyperechogenic mass in the right ovary (without positive growth dynamic) was a probable sign of recurrent dermoid cyst.
Discussion
Usually, dermoid ovarian cysts are asymptomatic and found accidentally during routine checkups, pregnancy, or surgery due to other reasons. Larger cysts can cause nonspecific lower abdominal pain, the most common symptom [14, 15]. Other symptoms include nausea and vomiting, breast enlargement, vaginal bleeding, menstrual disturbances (secondary amenorrhea or irregular menses) and hirsutism [4, 15, 16]. Occasionally, ovarian dermoids contain functioning pituitary tissue deriving from the ectoderm and have the potential to secrete hormones, such as prolactin or adrenocorticotropic hormone (ACTH) [17]. Excess prolactin in women can cause hypogonadism, oligomenorrhea, infertility, or galactorrhea, and ectopic ACTH production can result in acute weight gain, abdominal striae, and Cushing’s syndrome [17, 18]. There have also been reported a few cases of ovarian teratomas containing thyroid tissue [19, 20]. However, due to their rare occurrence, hormone-producing dermoid cysts are usually diagnosed postoperatively after pathological examination.
A dermoid ovarian cyst can most commonly be complicated with an ovarian torsion. Other, less common complications can be rupture, infection, and malignant transformation. A rupture can be triggered by various reasons, including prolonged pressure on the tumor (such as pregnancy or delivery of the fetus), direct trauma, or even internal pressure from the fast accumulation of cystic contents. In the worst possible situation, a cyst rupture can lead to massive spillage of the cystic contents into the peritoneal cavity, causing acute chemical peritonitis. On the other hand, if the leakage is slow and accumulates over time because of a small tear in the cyst’s wall, it could cause chronic granulomatous peritonitis [21].
Ultrasound (US) is the primary diagnostic tool for detecting dermoid ovarian cysts. Most teratomas show nonspecific findings on imaging. A dermoid plug, Rokitansky nodule, or floating balls sign findings on imaging are highly reliable radiographic evidence that supports a teratoma diagnosis [22]. Rokitansky nodule is characterized as a densely echogenic structure that often contains teeth, hair, and bony structures [23]. Computed tomography (CT) and magnetic resonance imaging (MRI) are alternative methods of diagnosing dermoid cysts [24]. CT scan continues to be the most requested modality of imaging, especially when abdominal pains are the main complaint of the patient. In CT images, mature teratoma typically manifests as high amounts of fat, fat-fluid/fluid-fluid level, calcifications, tufts of hair, and Rokitansky protuberance. It should be mentioned that CT or MRI are used only if the ultrasonographic appearance is not typical and that they help to remove the uncertainty of a teratoma diagnosis [25].
Treatment of dermoid ovarian cysts depends on the risk of malignancy, the age of the patient, and the need for fertility reserves. Usually, dermoid cysts grow slowly (1.8 mm a year) and do not need to be removed [26]. Symptomatic, larger than 5 cm, and atypical dermoids require surgery [27]. Surgeries like cystectomy and oophorectomy can be performed either laparoscopically or laparatomically. Nowadays, laparoscopy is the preferred tactic in the management of all benign ovarian masses [28]. Potential benefits of laparoscopy compared to traditional laparotomy include reduced postoperative pain, less blood loss, shorter recovery, fewer complications, and better cosmetic results [28, 29]. However, laparoscopic ovarian cystectomy can result in longer operating time, higher rate of contents spillage and higher rate of recurrence when compared with laparotomy [30, 31]. Laparotomy is recommended for teratomas greater than 10 cm [32]. Ovarian cystectomy is the usual choice in younger women with ovarian teratomas [28]. Postmenopausal and perimenopausal women with multiple cysts in the same ovary or with large ovarian teratoma usually do not have much ovarian tissue to conserve. Thus, oophorectomy is the optimal choice [33, 34]. Adolescents are a particularly challenging group to treat, as the patient’s sexual development and future fertility must be taken into account. Ovarian cystectomy is thought to be a safe procedure in terms of fertility preservation because it leaves enough viable ovarian follicles for future procreation [27]. Nevertheless, it was found that serum AMH (Anti-Mullerian Hormone, used to evaluate ovarian reserve concentration) decreased by 25% in women who underwent ovarian cystectomy [35]. The AMH decline was more prominent in women who experienced intraoperative bleeding, had endometriotic cysts, or had a more difficult dissection of the cyst [35]. Due to such recent findings, some scientists argue that the tactic of expectant management without intervention should always be considered in young adults. The benefit of preserving fertility outweighs the risk of recurrence or malignancy of small asymptomatic ovarian dermoids in adolescents [27].
After successful surgical management, benign ovarian teratomas have excellent prognosis with some risk of recurrence in 2 to 10 years. To avoid the recurrence of an ovarian teratoma, a laparoscopic approach should be discussed first since it is considered to have a lower chance of recurrence compared to other treatment tactics [28]. Another study found that young age (less than 30 years), large cyst size (greater than or equal to 8 cm), and bilateral cysts were significant predictive factors for recurrence [36].
Conclusions
Ovarian dermoid cysts are a common benign ovarian tumor, usually found incidentally. They are generally asymptomatic, occasionally presenting with abdominal pain or hormonal effects. The treatment strategy depends on many factors, but large, symptomatic cysts often require surgical management. Ovarian teratomas have a slight chance of recurrence.
References
1. Powell JK. Benign adnexal masses in the adolescent. Adolesc Med Clin 2004; 15(3): 535–547.
2. Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. Radiographics 2001; 21(2): 475–490.
3. Pekar-Zlotin M, Rabinovich I, Goldrat I, Vaknin Z, Gidoni Y, Zur-Naaman H, Maymon R, Smorgick N. Ovarian dermoid cysts associated with paraneoplastic syndrome N-methyl-D-aspartic acid receptor antibodies encephalitis. J Minim Invasive Gynecol 2021; 28(6): 1190–1193.
4. Ayhan A, Bukulmez O, Genc C, Karamursel BS, Ayhan A. Mature cystic teratomas of the ovary: case series from one institution over 34 years. Eur J Obstet Gynecol Reprod Biol 2000; 88(2): 153–157.
5. Masson E. EM-Consulte. In: Benign Gynecologic Lesions: Vulva, Vagina, Cervix, Uterus, Oviduct, Ovary. Available at <https://www.em-consulte.com/article/520024/benign-gynecologic-lesions-vulva-vagina-cervix-ute>.
6. Harada M, Osuga Y, Fujimoto A, Fujimoto A, Fujii T, Yano T, Kozuma S. Predictive factors for recurrence of ovarian mature cystic teratomas after surgical excision. European Journal of Obstetrics & Gynecology and Reproductive Biology 2013; 171(2): 325–328.
7. Comerci JT, Licciardi F, Bergh PA, Gregori C, Breen JL. Mature cystic teratoma: a clinicopathologic evaluation of 517 cases and review of the literature. Obstet Gynecol 1994; 84(1): 22–28.
8. Fayez I, Khreisat B, Athamneh T, Omoosh R, Daibes MA. Multiple bilateral ovarian mature cystic teratomas with ovarian torsion: a case report. Oman Med J 2018; 33(2): 163–166.
9. Newsom-Davis T, Poulter D, Gray R, Ameen M, Lindsay I, Papanikolaou K, Butler-Manuel S, Christmas T, Townsend P, Seckl M. Case report: malignant teratoma of the uterine corpus. BMC Cancer 2009; 9: 195.
10. Linder D, McCaw BK, Hecht F. Parthenogenic origin of benign ovarian teratomas. N Engl J Med 1975; 292(2): 63–66.
11. Plattner G, Oxorn H. Familial incidence of ovarian dermoid cysts. Canadian Medical Association Journal 1973; 108(7): 892.
12. Hegazy AA, Al-Qtaitat AI, Hegazy RA. A new hypothesis may explain human parthenogenesis and ovarian teratoma: a review study. IJRM 2023; 21(4): 277–284.
13. Keene DJB, Craigie RJ, Shabani A, Batra G, Hennayake S. Bipartite anterior extraperitoneal teratoma: evidence for the embryological origins of teratomas? Case Reports in Medicine 2011; 2011: 208940.
14. Saleh M, Bhosale P, Menias CO, Ramalingam P, Jensen C, Iyer R, Ganeshan D. Ovarian teratomas: clinical features, imaging findings and management. Abdom Radiol (NY) 2021; 46(6): 2293–2307.
15. Kirkham YA, Lacy JA, Kives S, Allen L. Characteristics and management of adnexal masses in a canadian pediatric and adolescent population. J Obstet Gynaecol Can 2011; 33(9): 935–943.
16. Templeman C, Fallat ME, Blinchevsky A, Hertweck SP. Noninflammatory ovarian masses in girls and young women. Obstet Gynecol 2000; 96(2): 229–233.
17. Ovarian teratoma with pituitary tissue: a case report. PMC. Available at <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7750138/>.
18. Huang B, Wu X, Zhou Q, Hu Y, Zhao H, Zhu H, Zhang Q, Zheng F. Cushing’s syndrome secondary to ectopic ACTH secretion from carcinoid tumor within an ovarian mature teratoma: a case report and review of the literature. Gynecol Endocrinol 2014; 30(3): 192–196.
19. Medić F, Miletić AI, Jakovčević A, Habek D. Papillary thyroid carcinoma within a mature cystic ovarian teratoma. Wien Med Wochenschr 2023; 173(9): 245–247.
20. Dane C, Ekmez M, Karaca A, Ak A, Dane B. Follicular variant of papillary thyroid carcinoma arising from a dermoid cyst: a rare malignancy in young women and review of the literature. Taiwanese Journal of Obstetrics and Gynecology 2012; 51(3): 421–425.
21. Takeda A, Koike W. Clinical characteristics and laparoscopic surgical outcomes of ovarian dermoid cysts complicated by spontaneous rupture: nine cases and a literature review. J Int Med Res 2023; 51(5): 03000605231171023.
22. Abdelmoaty MA, Taha WS. Pediatric puzzle: large ovarian dermoid cyst and markedly elevated CA 19-9 in an 8-year-old. Qatar Med J 2024; 2024(3): 47.
23. Mazhoud I, Skhiri W, Hafsa C, Toumi D, Maatouk M, Ben Salem A. Ruptured mature ovarian teratoma: a case report. Int J Surg Case Rep 2022; 102: 107788.
24. Kite L, Uppal T. Ultrasound of ovarian dermoids – sonographic findings of a dermoid cyst in a 41-year-old woman with an elevated serum hCG. Australasian J Ultrasound Med 2011; 14(3): 19–21.
25. Gürel H, Gürel SA. Ovarian cystic teratoma with a pathognomonic appearance of multiple floating balls: a case report and investigation of common characteristics of the cases in the literature. Fertility and Sterility 2008; 90(5): 2008.
26. Caspi B, Appelman Z, Rabinerson D, Zalel Y, Tulandi T, Shoham Z. The growth pattern of ovarian dermoid cysts: a prospective study in premenopausal and postmenopausal women. Fertil Steril 1997; 68(3): 501–505.
27. O’Neill KE, Cooper AR. The approach to ovarian dermoids in adolescents and young women. J Pediatr Adolesc Gynecol 2011; 24(3): 176–180.
28. Sinha A, Ewies AAA. Ovarian mature cystic teratoma: challenges of Surgical Management. Obstet Gynecol Int 2016; 2016: 2390178.
29. Lin P, Falcone T, Tulandi T. Excision of ovarian dermoid cyst by laparoscopy and by laparotomy. Am J Obstet Gynecol 1995; 173(3 Pt 1): 769–771.
30. Benezra V, Verma U, Whitted RW. Comparison of laparoscopy versus laparotomy for the surgical treatment of ovarian dermoid cysts. Gynecol Surg 2005; 2(2): 89–92.
31. Laberge PY, Levesque S. Short-term morbidity and long-term recurrence rate of ovarian dermoid cysts treated by laparoscopy versus laparotomy. J Obstet Gynaecol Can 2006; 28(9): 789–793.
32. Chang CK, Teng SW, Leu FJ. Laparoscopy versus laparotomy for cystic ovarian teratomas. Int J Gynaecol Obstet 2005; 88(1): 69–70.
33. Howard FM. Surgical management of benign cystic teratoma. Laparoscopy vs. laparotomy. J Reprod Med 1995; 40(7): 495–499.
34. Anteby EY, Ron M, Revel A, Shimonovitz S, Ariel I, Hurwitz A. Germ cell tumors of the ovary arising after dermoid cyst resection: a long-term follow-up study. Obstet Gynecol 1994; 83(4): 605–608.
35. Lind T, Hammarström M, Lampic C, Rodriguez-Wallberg K. Anti-Müllerian hormone reduction after ovarian cyst surgery is dependent on the histological cyst type and preoperative anti-Müllerian hormone levels. Acta Obstet Gynecol Scand 2015; 94(2): 183–190.
36. Fibus TF. Intraperitoneal rupture of a benign cystic ovarian teratoma: findings at CT and MR imaging. AJR Am J Roentgenol 2000; 174(1): 261–262.
Author Contributions
Aušrinė Anužytė: investigation, formal analysis, writing – original draft.
Eglė Noreikaitė: investigation, formal analysis, writing – original draft.
Viktorija Žitkutė: writing – review and editing.
Linas Andreika: consulting, writing – review and editing.