Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(2), pp. 120–125 DOI: https://doi.org/10.15388/LietChirur.2025.24(2).5
Primary Non-Hodgkin Lymphoma of the Temporal Bone: Case Report
Rokas Trainavičius
Vilniaus universitetas, Medicinos fakultetas, Klinikinės medicinos institutas,
Ausų, nosies, gerklės ir akių ligų klinika, Vilnius, Lietuva
Vilnius University, Faculty of Medicine, Institute of Clinical Medicine,
Clinic of Ear, Nose, Throat and Eye Diseases, Vilnius, Lithuania
E-mail: rokas.trainavicius@mf.vu.lt
https://ror.org/03nadee84
Saulė Sinkevičiūtė
Vilniaus universitetas, Medicinos fakultetas, Vilnius, Lietuva
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
E-mail: saule.sinkeviciute@mf.stud.vu.lt
https://ror.org/03nadee84
Abstract. Lymphomas account for approximately 2.5% of head and neck malignancies, with primary temporal bone involvement being exceedingly rare. The diagnosis of lymphoma, as with other temporal bone malignancies, is often delayed, which adversely impacts both treatment outcomes and overall prognosis. We report a case of a 55-year-old male who presented to our hospital with left-sided facial palsy, unilateral hearing loss, and auricular pain. Biopsies taken during surgical intervention revealed diffuse large B-cell lymphoma infiltrating the mastoid process, external auditory canal, and tympanic cavity. This case underscores the diagnostic challenges posed by temporal bone lymphoma, particularly in presenting symptoms that mimic benign conditions. It emphasizes the importance of considering malignancy in patients with persistent otological symptoms and facial nerve palsy, warranting thorough investigation. Maintaining a heightened level of suspicion for neoplastic disease is crucial until a definitive diagnosis is confirmed. Early detection through comprehensive imaging and biopsy is essential for effective management and improved outcomes.
Keywords: lymphoma, Non-Hodgkin lymphoma, temporal bone malignancies.
Pirminė ne Hodžkino limfoma smilkinkaulyje: klinikinio atvejo aprašymas
Santrauka. Limfomos sudaro maždaug 2,5 proc. visų galvos ir kaklo piktybinių navikų, tačiau pirminis smilkinkaulio pažeidimas itin retas. Kaip ir kitų smilkinkaulio piktybinių darinių, limfomos diagnozė dažnai nustatoma pavėluotai, o tai daro neigiamą įtaką gydymo rezultatams ir prognozei. Straipsnyje aprašomas 55 m. vyro klinikinis atvejis. Pacientas atvyko į ligoninę dėl kairės pusės veido parezės, suprastėjusios klausos kaire ausimi ir kairės ausies skausmo. Operacijos metu paimta biopsinė medžiaga patvirtino difuzinę didelių B ląstelių limfomą, infiltruojančią speninę ataugą, išorinę klausomąją landą ir būgninę ertmę. Šis atvejis pabrėžia smilkinkaulio limfomos diagnostinius iššūkius, ypač kai klinikiniai požymiai primena nepiktybinius susirgimus. Pacientams, kuriems pasireiškia išliekantys otologiniai simptomai kartu su veidinio nervo pažeidimu, būtina atlikti išsamius diagnostinius tyrimus ir neatmesti piktybinio proceso tikimybės, kol bus patvirtinta galutinė diagnozė. Ankstyva diagnostika, taikant pažangius vaizdinius ir histologinius tyrimus, yra esminė, siekiant taikyti tinkamiausią gydymą ir užtikrinti geresnes išeitis.
Reikšminiai žodžiai: limfoma, ne Hodžkino limfoma, smilkinkaulio piktybiniai dariniai.
Received: 2025 02 13. Accepted: 2025 03 14.
Copyright © 2025 Rokas Trainavičius, Saulė Sinkevičiūtė. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Lymphomas are malignant monoclonal proliferations of lymphoid cells. They comprise approximately 2.5% of head and neck malignancies and rank as the second most common neoplasm in this region after squamous cell carcinoma [1, 2]. Malignancies involving the temporal bone are exceedingly rare, comprising less than 0.2% of all head and neck cancers [1–3]. These cases pose diagnostic challenges due to their non-specific symptoms, which mimic benign otologic conditions [1, 4].
This report discusses a case of diffuse large B-cell lymphoma with temporal bone involvement, highlighting diagnostic strategies and treatment implications in managing such unusual presentations.
Case Report
A 55-year-old man was referred to our hospital’s emergency department following one month of unsuccessful treatment at another facility. The patient presented with ear pain, hearing loss, and facial weakness, all localized to the left side. According to the patient, his symptoms had begun approximately a month earlier, prompting him to seek medical care. During the initial examination, swelling of the external auditory canal and purulent discharge were observed, obscuring the view of the eardrum. Local antibiotics and non-steroidal anti-inflammatory drugs were prescribed, but the symptoms persisted, leading the patient to seek further medical attention. It was then decided to hospitalize him and administer intravenous antibiotics. Despite continued hospital treatment, the symptoms persisted, and facial weakness developed on the left side. Given the ineffective response to intravenous antibiotics and the new onset of facial paresis, a computed tomography (CT) scan was conducted. The CT scan revealed opacified mastoid air cells and fluid in the tympanic cavity (Figure 1). Due to the patient’s deteriorating condition, he was referred to a tertiary hospital for consultation with an otorhinolaryngologist.
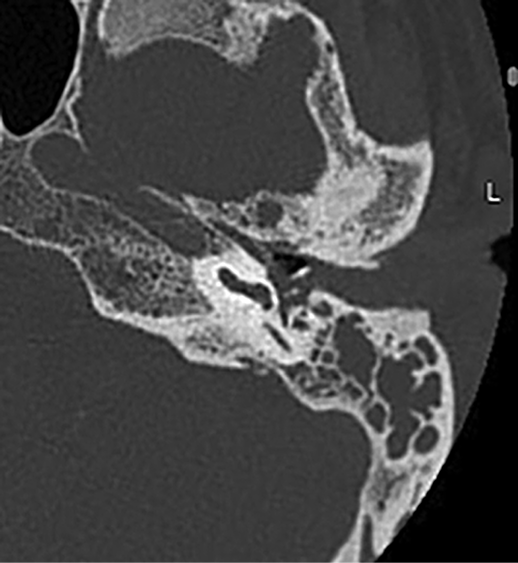
Figure 1. CT scan (axial view) of the temporal bone demonstrates opacification of the left mastoid air cells, tympanic cavity, and external auditory canal
Otoscopic examination revealed a swollen and obstructed left external auditory canal, preventing visualization of the tympanic membrane. Palpation of the auricle and the mastoid process was non-tender. Clinical examination demonstrated left-sided facial nerve palsy, characterized by ptosis of the left corner of the mouth and incomplete closure of the left eyelid.
Laboratory investigations indicated an elevated white blood cell count (WBC: 12.46×109/L) and elevated C-reactive protein (CRP: 14.6 mg/L).
Due to the development of facial palsy despite conservative treatment, the medical team opted for surgical exploration of the middle ear. A canal wall down mastoidectomy was performed, accompanied by decompression of the facial nerve. During the operation, pathological masses were observed in the mastoid process, external auditory canal, and tympanic cavity, prompting the team to take biopsies.
The surgery and postoperative period proceeded without complications. Following the operation, the patient was treated with intravenous antibiotics and prednisone. The ear pain resolved though left-sided hearing loss and facial nerve palsy persisted. The patient was discharged one week later to continue treatment in an outpatient setting.
Pathological examination of all samples from the external auditory canal, mastoid air cells, and tympanic cavity confirmed diffuse large B-cell lymphoma (DLBCL). Based on these findings, the patient was urgently referred for consultation with a hematologist.
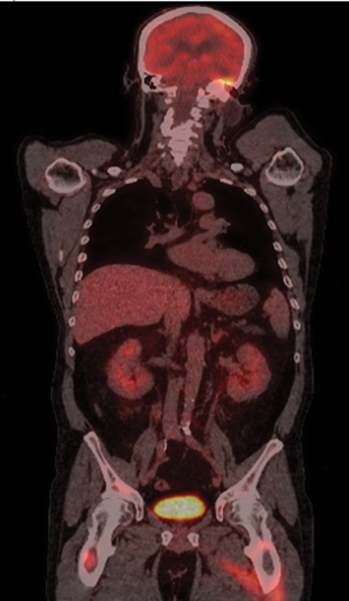
Figure 2. Whole-body PET scan (coronal view) reveals hypermetabolic foci in the petrous pyramid of the left temporal bone, with radiotracer accumulation in the brain, mediastinum, adrenal glands, pancreas, kidneys, and multiple bone lesions, particularly in the femurs
A whole-body fluorodeoxyglucose positron emission tomography (PET) scan was conducted. The PET scan revealed extensive disease involvement in the left petrous pyramid and widespread disease across various other organs and bones (Figure 2). These findings were consistent with Lugano stage IV lymphoma.
A magnetic resonance imaging (MRI) study of the brain was performed. The imaging results revealed intracranial lymphomatous masses localized within the left side of the temporal basal region (Figure 3).
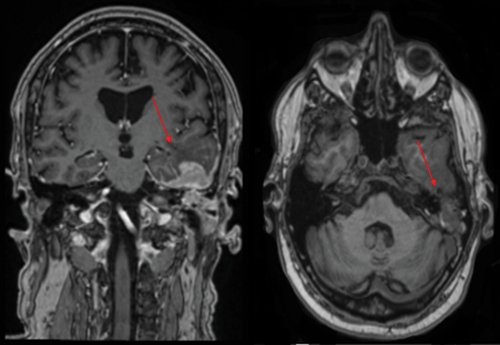
Figure 3. MRI scans of the brain (coronal and axial view). Arrows showing intracranial lymphomatous masses in the left temporal basal region, involving the left petrous pyramid and mastoid process
Following biopsy confirmation and diagnosis of DLBCL, the patient underwent multiple chemotherapy cycles in the hematology department and was placed under routine surveillance for follow-up. Periodic assessments by otorhinolaryngologists were also conducted. While the ear’s condition remained stable, as confirmed by multiple MRI scans, the disease unfortunately showed significant systemic spread. This progression led to a deterioration in other body regions, ultimately resulting in the patient’s death due to the widespread disease.
Discussion
Lymphoma is a malignancy of the reticuloendothelial system and exhibits a notable prevalence in the head and neck region, with an incidence rate of approximately 2.5% [1, 2, 4]. Lymphomas can affect various anatomical sites, including Waldeyer’s ring, nasal cavity, paranasal sinuses, salivary glands, thyroid gland, and orbit [1]. Non-Hodgkin’s lymphoma (NHL) represents the most common subtype of head and neck lymphomas, with the majority being classified as B-cell lymphomas [5]. NHL typically presents with cervical lymph node involvement, but in 40% of the cases, extranodal sites may be the primary location of the disease [6].
While involvement of the temporal bone is rare, it does occur [5]. Primary lymphoma originating in the temporal bone usually involves the mastoid and middle ear, with involvement of the external and internal auditory canals occurring less frequently [1–3]. A layer of lymphoid tissue situated within the mucosal epithelium of the mastoid antrum, tympanic cavity, and tympanic opening of the eustachian tube serves as the primary site of origin for the lymphoma [2]. This malignancy can occur across all age groups but shows a tendency to present in adults, with a male predominance. The male-to-female ratio typically ranges from 1.5 to 2:1 [1, 7].
The clinical presentation of primary temporal bone lymphoma is highly non-specific. Early diagnosis can be particularly challenging due to the complex anatomy of the middle ear and the overlap in clinical presentation with benign conditions. Common symptoms, such as otalgia, hearing loss, otorrhea, aural fullness, and tinnitus, often resemble those of non-malignant pathologies. As a result, these malignant disorders are frequently misdiagnosed and erroneously treated as external or middle ear otitis, complicating timely detection and leading to inappropriate treatment [1, 4, 6]. Temporal bone lymphoma diagnosis should always be considered in cases of infections resistant to standard treatment protocols [1].
As the lesion progresses, clinical signs may include progressive hearing loss, severe otalgia, a palpable mass, otorrhagia, or facial nerve palsy [1, 3, 6]. Facial nerve palsy is a rare complication of lymphoma, primarily due to the resistance of the nerve sheath to neoplastic infiltration. This condition results from the destruction of the bony facial canal by the tumor, allowing direct invasion of the nerve fibers by malignant cells. Tumor involvement of the facial nerve most commonly occurs in the region of the geniculate ganglion, as observed in our case [1, 2]. Facial nerve weakness is usually an advanced sequela of middle ear pathology that warrants consideration of more serious underlying conditions and necessitates more aggressive treatment [3, 4].
High-resolution computed tomography and magnetic resonance imaging are critical for a comprehensive assessment of malignancies involving the temporal bone, with contrast-enhanced MRI additionally providing important information regarding perineural spread along the facial nerve [1, 2]. Any radiologic findings deemed abnormal and raising suspicion for a neoplasm should be subjected to biopsy for further evaluation [1]. Histopathology and immunohistochemical profiling are essential for developing a targeted chemotherapeutic strategy tailored to the specific characteristics of the malignancy. Additionally, positron emission tomography-computed tomography is vital for staging the disease, identifying extratemporal pathologies, and monitoring the response to therapy [2]. Patients should undergo chemotherapy and may warrant closer follow-up for tumor recurrence and disease progression [3].
Conclusions
Temporal bone lymphoma is an exceedingly rare condition that poses considerable diagnostic challenges in contemporary clinical practice, with the existing literature documenting a limited number of cases. This malignancy often presents with symptoms resembling those of more prevalent benign ear pathologies, complicating the diagnostic process. Common presenting symptoms are typically non-specific and may indicate advanced inflammatory processes, thereby obscuring the recognition of underlying malignancies. In instances of persistent or severe symptoms, such as facial palsy, a malignant etiology should be considered, necessitating prompt imaging of the temporal bone to facilitate early detection and appropriate management. Although the incidence of temporal bone cancer remains low, it is imperative to maintain a high index of suspicion for neoplastic disease in patients exhibiting these symptoms until a definitive diagnosis is attained.
References
1. Kaoutar C, Ahmedou AB, Youssef O, Sami R, Abada R, Mohamed R, Mohamed M. Primary Non-Hodgkin lymphoma of the temporal bone: a rare case report. Annals of Medicine and Surgery 2021; 64: 102205. DOI: 10.1016/j.amsu.2021.102205.
2. Vaid S, Jadhav J, Chandorkar A, Vaid N. Bilateral Non-Hodgkin’s lymphoma of the temporal bone: a rare and unusual presentation. Case Reports in Otolaryngology 2016; 2016: 1–5. DOI: 10.1155/2016/2641876.
3. Uy JAG, Jugo JCZ, Acuin JM. Primary lymphoma of the temporal bone: the first locally reported case. Philippine Journal of Otolaryngology Head and Neck Surgery 2008; 23(2): 23–27. DOI: 10.32412/pjohns.v23i2.733.
4. Alqunaee M, Aldaihani A, AlHajery M. Non-Hodgkin’s lymphoma of the middle ear presenting as mastoiditis. Case Reports in Otolaryngology 2018; 2018: 1–4. DOI: 10.1155/2018/7639784.
5. Alvi SA, Flynn JP, Gener M, Cullen R. Burkitt lymphoma of the temporal bone. Otology & Neurotology 2018; 39(5): e410–e412. DOI: 10.1097/mao.0000000000001782.
6. Bruschini L, De Vito A, Fortunato S, Pelosini M, Cervetti G, Petrini M, Berrettini S. A case of primary Non-Hodgkin’s lymphoma of the external auditory canal. Case Reports in Otolaryngology 2013; 2013: 1–4. DOI: 10.1155/2013/138397.
7. Ogawa S, Tawara I, Ueno S, Kimura M, Miyazaki K, Nishikawa H, Yamaguchi M, Kobayashi T, Shiku H. De novo CD5-positive diffuse large B-cell lymphoma of the temporal bone presenting with an external auditory canal tumor. Internal Medicine 2006; 45(11): 733–737. DOI: 10.2169/internalmedicine.45.1671.
Author Contributions
Rokas Trainavičius: Conceptualization, Clinical Management, Data Collection, Writing – Original Draft, Writing – Review & Editing, Supervision.
Saulė Sinkevičiūtė: Conceptualization, Data Collection, Writing – Original Draft, Writing – Review & Editing. All authors: Approval of Final Manuscript.