Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(3), pp. 232–238 DOI: https://doi.org/10.15388/LietChirur.2025.24(3).8
Navigating the Enigma of Parathyroid Adenoma ‒ a Tale of Diagnosis, Surgery, and Skeletal Symphony
Agniban Chakraborty
Armed Forces Medical College, Department of General Surgery, Pune, Maharashtra, India
E-mail: dr.agnibanchakraborty@gmail.com
https://orcid.org/0000-0002-5528-398X
https://ror.org/05g6w6j42
Arun Kumar
Armed Forces Medical College, Department of General Surgery, Pune, Maharashtra, India
E-mail: ak3.doc@gmail.com
https://orcid.org/0000-0002-6577-5937
https://ror.org/05g6w6j42
Vitesh Popli
Armed Forces Medical College, Department of General Surgery, Pune, Maharashtra, India
E-mail: vitesh03@gmail.com
https://orcid.org/0000-0002-8473-0662
https://ror.org/05g6w6j42
Ashok Kumar Ponnam
Armed Forces Medical College, Department of General Surgery, Pune, Maharashtra, India
E-mail: ashponnam95@gmail.com
https://orcid.org/0009-0009-6827-6031
https://ror.org/05g6w6j42
Sidhartha Goutam
Armed Forces Medical College, Department of General Surgery, Pune, Maharashtra, India
E-mail: hell.hellboy8@gmail.com
https://orcid.org/0009-0006-2492-2984
https://ror.org/05g6w6j42
Abstract. Parathyroid adenomas, though uncommon, can pose significant challenges in diagnosis and management due to their elusive nature. We present a case report of a 47-years old female who presented with a constellation of symptoms indicative of hyperparathyroidism. Initial laboratory investigations revealed elevated serum calcium levels, corroborated by an increased parathyroid hormone (PTH) level. Further imaging studies, including neck ultrasonography and technetium-99m sestamibi scintigraphy, identified a solitary parathyroid adenoma. The patient’s clinical history, coupled with imaging findings, guided surgical approach towards a minimally invasive parathyroidectomy.
Histopathological examination of the excised adenoma confirmed the diagnosis, displaying characteristic features of parathyroid tissue hyperplasia. Postoperatively, the patient experienced a rapid normalization of serum calcium and PTH levels, accompanied by a resolution of symptoms. This case underscores the importance of a multidisciplinary approach in the diagnosis and management of parathyroid adenomas, emphasizing the pivotal role of advanced imaging techniques in localizing these elusive lesions.
Additionally, it highlights the efficacy of minimally invasive surgical interventions in achieving successful outcomes with reduced morbidity. The presented case contributes to the existing body of knowledge on parathyroid adenomas, providing insights into their clinical presentation, diagnostic challenges, and the significance of timely intervention. Improved awareness and understanding of such cases are crucial for optimizing patient outcomes and refining diagnostic and therapeutic strategies for this rare endocrine disorder.
Keywords: parathyroid adenoma, hyperparathyroidism, PTH.
Received: 2025-03-12. Accepted: 2025-05-14.
Copyright © 2025 Agniban Chakraborty, Arun Kumar, Vitesh Popli, Ashok Kumar Ponnam, Sidhartha Goutam. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Hyperparathyroidism (HPT) refers to excess synthesis and secretion of Parathyroid hormone (PTH) by abnormal parathyroid glands. Depending on the underlying cause, HPT is classified as primary, secondary, or tertiary. Primary HPT is caused by autonomous overproduction of PTH by one or more abnormal parathyroid glands. Most patients with primary HPT present with hypercalcemia and an elevated or inappropriately high-normal (nonsuppressed) PTH level. It affects 1 out of every 500 women and 1 out of every 2 000 men [1]. Primary HPT and malignancy are the most common causes of hypercalcemia in adults, accounting for approximately 80% of all cases of hypercalcemia [1]. Primary HPT occurs when one or more abnormal parathyroid glands enlarge and secrete PTH inappropriately relative to serum calcium levels. The three pathologic conditions that result in primary HPT are parathyroid adenoma, hyperplasia, and carcinoma.
Parathyroid adenomas are benign neoplasms of the parathyroid glands, constituting a major cause of primary hyperparathyroidism. Increased serum calcium levels occur as a result of PTH-induced increase in bone resorption, renal calcium reabsorption, and indirectly by increased dietary calcium absorption from the gastrointestinal tract. Up to 80% of patients with primary HPT are diagnosed as a result of incidental hypercalcemia found on routine bloodwork [2]. However, patients with primary HPT can have diverse symptoms, which are the result of calcium effects on multiple organ systems, including the renal, skeletal, gastrointestinal, cardiac, and neuromuscular systems. In a recent cohort study of over 9 000 patients, 35% of patients had objective findings of end-organ effects at the time of diagnosis, including osteoporosis, nephrolithiasis, or hypercalciuria. In addition, 62% of patients developed end-organ effects within 5 years of diagnosis [3].
Primary HPT results in loss of bone mass, which is most pronounced at sites of cortical bone in the distal third of the radius and the femoral neck [4]. Up to 15% of patients with HPT have osteopenia in the lumbar spine and 35% for distal radius [5].
This case report aims to elucidate the diagnostic challenges, clinical manifestations, and successful management of a patient of parathyroid adenoma Primary Hyperparathyroidism.
Case report
A 47 years old lady, a known case of rheumatoid arthritis (not on any medications), presented with complains of progressive low back ache along with multiple joint pains for 4 years duration and pain over left hip with difficulty in walking for 1 year duration. The pain was insidious in onset and gradually progressed to severe intensity leading to restriction in ambulation. She also gave a history of chronic constipation since 1 year and altered sleep patterns for 3 months duration.
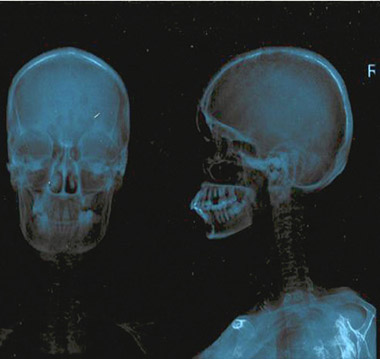
The patient had suffered trivial trauma to hip when she fell down in bathroom 3 months prior to presentation and she has been wheelchair bound since then. She was initially evaluated at a private hospital and was diagnosed as a case of pathological fracture of neck of left femur. Initial X-Ray skull, pelvis and LS spine revealed salt and pepper appearance, osteopenia with osteophytes and decreased L3‒L4 & L4‒L5 disc spaces (Figures 1A, 1B).
|
|
|
|
A. Salt pepper appearance of skull |
B. Multiple osteolytic lesion in skeletal bones, pelvis and LS spine |
|
Figure 1. |
|
She was thereafter evaluated with MRI which showed prolapsed intervertebral discs (PIVD) at multiple cervical and lumbar levels with evidence of cord compression. There was an osseous lesion noted on the bilateral iliac bones, left proximal femur and ribs. Further she underwent PET CT which revealed lytic lesion in neck of bilateral femur, pelvic bone, sternum, ribs, left clavicle, scapula and skull. Fracture neck of Left femur neck was noted along with features suggestive of impending fracture neck of right femur. Her PTH level was found to be elevated (511.50 pg/ml) and thereafter she reported to this centre for further management.
On presentation, clinical examination revealed no significant findings. There was no evidence of any neck swelling. However, patient had hypercalcemia (11.1 mg/dl) and raised Alkaline Phosphatase (ALP) value (476 IU/L). On imaging, Ultrasonography (USG) of neck revealed a well defined round lesion in the left postero inferior thyroid lobe with vascularity, suggestive of parathyroid adenoma.
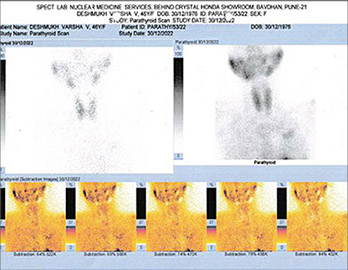
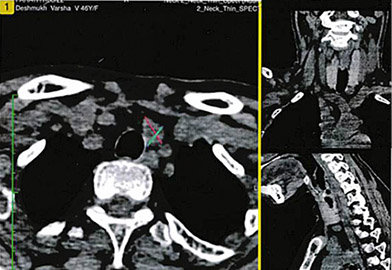
She was further evaluated with Sestamibi scan which confirmed a left inferior parathyroid adenoma of size 15x12x8 mm, abutting the inferior pole of left lobe of thyroid gland (Figure 2). Bone marrow biopsy from iliac crest lesion was suggestive of brown tumor of hyperparathyroidism as well. Dual energy X-ray absorptiometry (DEXA) or bone density scan was done to assess the severity and was suggestive of severe osteopenia at spine (Z score ‒4.9) and femur neck (Z score ‒4.5).
Following all workup, the final diagnosis was reached as “primary hyperparathyroidism with left inferior parathyroid adenoma with pathological fracture of left femur neck, impending fracture of right femur neck and PIVD of multiple cervical and lumbar disc levels with multiple brown tumors of hyperparathyroidism”.
Patient was thereafter planned for surgery. Pre-operatively she was given IV Zolendronic acid to reduce the risk of “hungry bone syndrome” in the post op period.
She underwent focussed neck exploration via minimally invasive approach under GA. Intra-operatively (findings as shown in Figures 3‒5), a nodular lesion was noted over left inferior thyroid gland. In view of suspected intra thyroid ectopic location of parathyroid, a left hemithyroidectomy was done. Intra-operative frozen Section was sent, however there was no parathyroid gland visualised in the excised tissue. Incision was then extended inferiorly and on further exploration, left inferior parathyroid lesion of size 1.5×1.5 cm was found at the intra-thymic location, which was confirmed by repeat frozen section after excision. Left recurrent laryngeal nerve (RLN) and left external laryngeal nerve (ELN) were seen and preserved.
|
|
|
|
A. Axial uptake image |
B. Transverse view – parathyroid marked with green-red cross |
|
Figure 2. Sestamibi scan showing left inferior parathyroid adenoma |
|
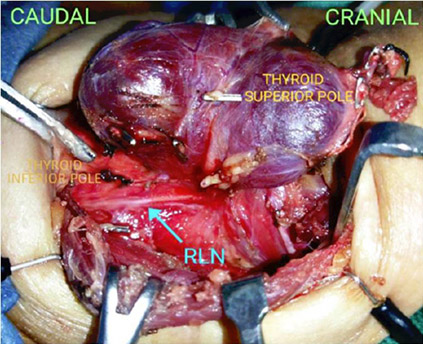
Figure 3. Focussed neck exploration showing relevant anatomy – the thyroid gland, left Recurrent laryngeal nerve (RLN), nodular lesion over inferior pole of left thyroid
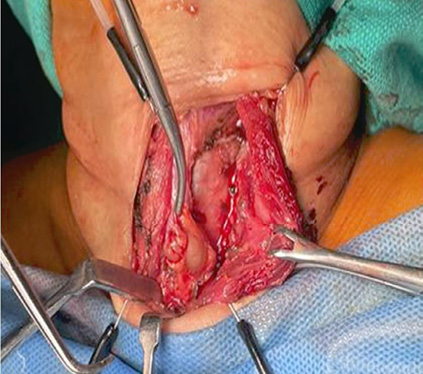
Figure 4. Intra-thymic Left inferior parathyroid – seen after left hemithyroidectomy
Intra-operative PTH (IOPTH) levels at 3 and 5 minutes post excision were noted as 129.1 pg/ml and 32.4 pg/ml respectively, which fulfilled the Miami Criteria (pre-incision level of PTH ‒ 511.10 pg/ml) and surgical endpoint was achieved.
Post operatively, she was monitored in the ICU for 24 hrs. Patient was started on oral calcium supplements and monitored 6 hourly for hypocalcemia as per IOWA guidelines. However, following 4 successive reports showing normal corrected calcium levels (8.8–9.24 mg/dl), calcium monitoring was stopped and patient was started on Vit D3 in addition to the calcium supplements.

Figure 5. Left inferior parathyroid gland after excision
PTH levels in post operative evening was found to be 0.01 pg/ml and the patient was started on Inj Teriparatide 20 mg via subcutaneous route once daily after shifting to general ward next day. She showed no features of hypocalcemia in the post op period and surgical wound was reviewed on Post-operative day (POD) 2 followed by staples removal on POD-07.
On histopathological examination, sections from left hemithyroidectomy revealed features of lymphocytic thyroiditis and left parathyroid specimen was consistent with parathyroid adenoma.
Following an uneventful post-op recovery, she was discharged with advice to follow up at orthopedics department for opinion regarding fixation of femur fracture 4 weeks after surgery, 6 monthly follow up with DXA scan and continue Inj Teriparatide for 2 years.
On follow up at 6 months, the patient has shown significant symptomatic improvement in terms of generalized weakness, pain and sleep patterns. She is now planned for DXA scan following which femur fracture will be managed surgically.
Discussion
Parathyroid adenomas are typically solitary, benign tumors that cause excessive secretion of PTH, leading to hypercalcemia. Clinical manifestations may include fatigue, nephrolithiasis, and bone pain. Prompt diagnosis is crucial to prevent complications such as renal calculi and osteoporosis. Surgical resection, often performed using minimally invasive techniques, remains the definitive treatment for parathyroid adenomas.
The presented case underscores the clinical complexity and challenges associated with the management of parathyroid adenoma, a rare but impactful cause of hypercalcemia. The discussion will delve into several key aspects, including the clinical presentation, diagnostic workup, surgical intervention, and the broader implications for patient care.
The patient’s initial complaints of bone pain, fatigue followed by sleep disturbances are characteristic of primary hyperparathyroidism, aligning with the known symptoms associated with elevated serum calcium levels. Parathyroid adenomas are often asymptomatic, making their diagnosis challenging. In this case, symptomatic presentation prompted a thorough investigation, leading to the identification of hypercalcemia and increased parathyroid hormone (PTH) levels.
Accurate and timely diagnosis is critical in managing parathyroid adenomas effectively. Radiological imaging, including neck ultrasound and technetium-99m sestamibi scintigraphy, played a crucial role in localizing the lesion to the left inferior parathyroid gland. DEXA scan revealed reduced bone mineral density, highlighting the potential impact of prolonged hypercalcemia on skeletal health.
Focussed neck exploration via minimally invasive approach followed by parathyroidectomy, guided by IOPTH monitoring, proved to be a successful intervention in this case. The prompt reduction in serum calcium levels postoperatively, coupled with the patient’s symptomatic improvement, highlights the effectiveness of surgical resection in managing hyperparathyroidism due to adenomas. The use of intraoperative PTH monitoring is a valuable adjunct in confirming the adequacy of the resection and ensuring the normalization of PTH levels. Pre-operative Zolindronate was done to reduce risk of “hungry bone syndrome” which often leads to sudden severe life-threatening hypocalcemia in immediate post-operative period.
The favorable postoperative course, characterized by sustained normalization of serum calcium and PTH levels, reinforces the curative nature of parathyroidectomy in the setting of parathyroid adenoma. The repeat DEXA scan on subsequent follow-up will bring out the importance of timely intervention in preventing long-term complications such as osteoporosis.
Conclusion
This case report highlights the successful management of hyperparathyroidism secondary to parathyroid adenoma through focused neck exploration and parathyroidectomy. This case report also brings out that parathyroid gland can present with an intra-operative surprise due to its variable possible locations. Intra-thymic location being an unusual site, the role of intra-operative frozen section and IOPTH monitoring to determine the surgical endpoint is invaluable. The timely diagnosis, accurate localization, and effective surgical intervention resulted in the normalization of serum calcium levels and improved bone health. While this case contributes to the existing literature, ongoing research is warranted to further refine our understanding of parathyroid adenomas and optimize patient care.
Authors contribution
Agniban Chakraborty ‒ conceptualization, methodology, formal analysis, investigation, writing ‒ original draft, visualization;
Arun Kumar ‒ conceptualization, methodology, formal analysis, writing ‒ review and editing;
Vitesh Popli ‒ conceptualization, methodology, formal analysis, writing ‒ review and editing;
Ashok Kumar Ponnam ‒ methodology, formal analysis, investigation, writing ‒ visualisation, review and editing;
Sidhartha Goutam ‒ methodology, formal analysis, investigation, writing ‒ visualisation, review and editing.
References
1. The parathyroid glands. In: Sabiston Textbook of Surgery, 21st ed., 2022; 921‒940.
2. The parathyroid glands. In: Bailey & Love’s Short Practice of Surgery, 28th ed., 2023; 873‒887.
3. Assadipour Y, Zhou H, Kuo EJ, Haigh PI, Adams AL, Yeh MW. End-organ effects of primary hyperparathyroidism: a population-based study. Surgery 2019; 165(1): 99‒104.
4. Insogna KL. Primary hyperparathyroidism. N Engl J Med 2018; 379(11): 1050‒1059.
5. Rubin MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E, Siris E, Udesky J, Silverberg SJ. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab 2008; 93(9): 3462‒3470.
6. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, Doherty GM, Herrera MF, Pasieka JL, Perrier ND, Silverberg SJ, Solórzano CC, Sturgeon C, Tublin ME, Udelsman R, Carty SE. The American Association of Endocrine Surgeons Guidelines for definitive management of primary hyperparathyroidism. JAMA Surg 2016; 151(10): 959‒968.
7. Udelsman R, Åkerström G, Biagini C, Duh QY, Miccoli P, Niederle B, Tonelli F. The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab 2014; 99(10): 3595‒3606.