Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(2), pp. 104–112 DOI: https://doi.org/10.15388/LietChirur.2025.24(2).3
Traumatic Brain Injury: A Study from the Middle-East
Muath Ibrahim Alfallaj
Qassim University, Department of Surgery, College of Medicine, Saudi Arabia
E-mail: MI.ALfallaj@qu.edu.sa
https://orcid.org/0009-0006-6174-4793
https://ror.org/01wsfe280
Sajad Ahmad Salati
Qassim University, Department of Surgery, College of Medicine, Saudi Arabia
E-mail: docsajad@gmail.com
https://orcid.org/0000-0003-2998-7542
https://ror.org/01wsfe280
Abstract. Background. Traumatic head injuries represent one of the major causes of mortality and long-term disability worldwide. This main objective of this study was to explore the patterns, severity, and outcomes of these injuries. Methods. An observational, descriptive, retrospective study was carried out utilizing a validated data collection sheet, after attaining a proper ethical committee approval. Well-defined exclusion and inclusion criteria were applied. Results. There were 185 patients enrolled in the study, including 153 (82.7%) males and 32 (47%) females, with a mean age of 41.5 years. Road traffic accidents were the most frequent cause of injury, followed by falls, machinery-related accidents, and assaults. A conservative strategy was used to treat 101 (54.6%) of the patients, whereas various surgical procedures were performed on 84 (45.4%). Outcomes were related to Glasgow Coma score on presentation and favorable in 135 (73%) patients. Conclusions. Road traffic accidents and falls from heights are the leading causes of traumatic brain injury. As a result, preventive measures including road safety and workplace regulations must be addressed.
Keywords: head injury, trauma, road traffic accident, fall, Glasgow Coma Scale, hematoma, outcomes.
Received: 2025 02 28. Accepted: 2025 03 28.
Copyright © 2025 Muath Ibrahim Alfallaj, Sajad Ahmad Salati. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Traumatic head injuries (THI) represent one of the leading causes of death and long-term disability between the ages of 18 and 44 in most countries [1]. It is a major public health and socioeconomic concern that requires ongoing monitoring of incidence, prevalence, and consequences. About 10 million people are estimated to suffer from THI annually worldwide which translates as 150–315 cases per 100,000 population [1, 2], and THI accounts for anywhere from a third to a half of over-all mortality from trauma [3]. The survivors may suffer from profound issues such as speech difficulty, personality changes, seizures, physical deformities, and cognitive impairments. Their rehabilitation places a strain on the family, the community, and the medical system.
According to estimates, the incidence of THI in Saudi Arabia is 116 per 100,000 people [4]. Multiple studies have been conducted in recent years in different regions of Saudi Arabia to understand the incidence, risk factors, treatment, outcomes, and healthcare needs of THI. A study conducted in the Riyadh region by Al-Habib et al. [5] revealed that about 70% of THIs were caused by road traffic accidents (RTA). A similar study from the Jeddah region [6] found RTA to be the most common cause of injury (61.4%), followed by falls (19.9%), whereas a study from the Aseer region [7] found RTA to be the cause of THI in 89.3%.
The goal of the current study, which was conducted in the Al-Qassim region of Saudi Arabia, was to characterize the clinical and demographic profiles of traumatic brain injury in adults to pinpoint the changeable traits that would be useful in recommending suitable therapeutic approaches. The research was completed in two phases:
1. Examining the general profile of traumatic head damage.
2. Examining the profiles of specific disorders, such as traumatic subarachnoid hemorrhage, acute subdural hemorrhage, and extradural hematoma.
The data pertaining to the study’s first phase is presented in this article.
Methods
An observational, descriptive study was conducted retrospectively at a tertiary care center in Al-Qassim region of Saudi Arabia, using a pre-tested validated data collection form. Patients’ enrolment was based on inclusion/exclusion criteria, and data related to the demographics and injury were retrieved from the electronic databank. The inclusion criteria included patients older than 18 years who were managed as inpatients after head injury from January 2022 to June 2023. The exclusion criteria included patients aged below 18 years or else suffering from any pre-existing neurological disorders such as cerebrovascular disease, cerebral space-occupying lesions, neuropathies, and dementia.
The outcome was assessed based on the Glasgow Coma Outcome Scale (GOS) as depicted in Figure 1. For simplification, GOS1 and GOS2 were categorized as unfavourable outcomes and GOS3-5 as favourable outcomes for simplification, based on the previously published series by Mauritz et al. [8].
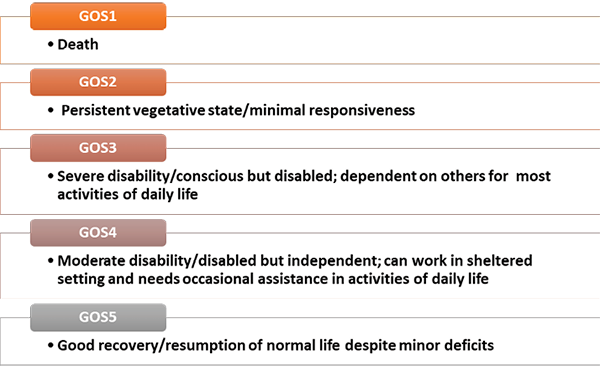
Figure 1. Glasgow Coma Outcome Scale (GOS)
The data were entered into a Microsoft Excel 2021 sheet and exported to SPSS (Statistical Package for Social Sciences) v ersion 26 for further analysis. Chi-square tests assessed associations between categorical variables (e.g., gender, type of injury, mechanism), while t-tests analyzed continuous variables like length of hospital stay. Odds ratio with 95% confidence intervals (CI) was computed to identify relations between the relevant variables, thereby setting statistical significance at p < 0.05.
Ethical considerations. The ethical committees of the Research and Studies at Qassim University and at Directorate of Health Affairs, Qassim cluster approved the current study. Patient-related data were preserved, and absolute confidentiality was maintained by exclusion of the identifying personal details in the analysis. The assigned protocol number is H/04/Q/001 and approval was released on 13 February 2023.
Results
Demographics. The study included 185 head injury patients, including 153 (82.7%) males and 32 (47%) females, ranging in age from 18 to 86 years (mean: 41.5±20.5 years), as depicted in Table 1. Eighty-seven (47%) of the patients were between the ages of 21 and 40.
Table 1. Patient characteristics (Demographics)
|
Variables |
Frequency (n = 185) |
Percentage |
|
|
Gender |
Female |
32 |
17.3 |
|
Male |
153 |
82.7 |
|
|
Age (years) |
<20 years |
22 |
11.9 |
|
21–40 years |
87 |
47.0 |
|
|
41–60 years |
35 |
18.9 |
|
|
61–80 years |
31 |
16.8 |
|
|
>80 years |
10 |
5.4 |
|
|
Mean (SD) |
41.5 (20.5) |
||
Mechanism of injury. Road traffic accidents were the commonest mode of injury (46%) as depicted in Table 2, and other causes included falls, machinery-related accidents, and assaults. On presentation to the emergency department, 136 (73.5%) patients had a Glasgow Coma Score (GCS) equal to or above 9, and 49 (26.5%) had scores equal to or lower than 8.
Table 2. Patient characteristics (Mechanism of Injury and Glasgow Coma Score)
|
Variable |
Category |
n |
Management |
Outcome |
||
|
S |
C |
Favourable |
Unfavourable |
|||
|
Mechanism |
Road traffic accidents |
85 |
41 |
44 |
53 |
32 |
|
Fall from height/construction site |
63 |
24 |
39 |
54 |
9 |
|
|
Machinery |
22 |
10 |
12 |
14 |
8 |
|
|
Assaults |
15 |
5 |
10 |
11 |
4 |
|
|
GCS Score on admission |
14–15 |
76 |
3 |
73 |
76 |
0 |
|
9–13 |
60 |
41 |
19 |
39 |
21 |
|
|
≤8 |
49 |
40 |
9 |
20 |
29 |
|
S – Surgical Management, C – Conservative Management
Imaging. All the patients underwent a non-contrast CT scan (with a bone window), and the findings (Table 3) included acute subdural hematoma (SDH), epidural hematoma (EDH), traumatic subarachnoid hemorrhage (SAH), skull fractures, contusions, and pneumocephalus. In 45 (24.3%) cases, CT scans showed a normal study.
Table 3. Patient characteristics (CT findings)
|
Category |
Frequency |
Percentage |
|
|
Imaging findings |
Acute Subdural Hemorrhage (SDH) |
63 |
34.1 |
|
Negative CT |
45 |
24.3 |
|
|
Epidural Hemorrhage (EDH) |
16 |
8.6 |
|
|
Subarachnoid Hemorrhage (SAH) |
10 |
5.4 |
|
|
Contusions/intracranial hematoma cerebral edema |
39 |
21.1 |
|
|
Linear Skull fractures |
8 |
4.3 |
|
|
Depressed skull fractures |
3 |
1.8 |
|
|
Pneumocephalus |
2 |
1.1 |
|
Management options. As depicted in Table 2, patients were managed by conservative/medical and surgical options. 84 (45.4%) cases underwent various surgical procedures, including intracranial pressure monitor insertion, evacuation of subdural/epidural hematomas, elevation of depressed skull fractures, and decompressive craniectomies, while 101 (54.6%) cases were managed with a conservative/medical approach ranging from observation in the neurosurgery ward to a full head injury protocol in which they received osmotic therapy, sedation, neuromuscular blockade, and optimization of blood pressure and oxygenation. Surgical intervention was required in 81 (43.7%) cases with GCS below 12, and only 3 (1.6%) with GCS 14 or 15 underwent surgical operation.
Outcomes. Outcomes as defined by GOS were favourable (GOS 3–5) in 135 (73%) cases and unfavourable (GOS 1, 2) in 50 (27%) cases. The outcomes had a statistically significant relationship (p < 0.05) with the GCS score of the patients at presentation in emergency and steadily deteriorated as the GCS decreased (Figure 2). Similarly, the outcomes were unfavourable in a greater number of patients admitted after road traffic accidents as compared to falls, machinery injuries, or assaults (p < 0.05).
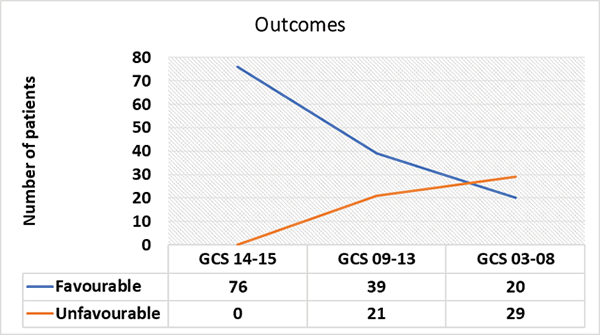
Figure 2. Relationship of outcomes after head injury to GCS score at presentation
Discussion
Several significant sociodemographic characteristics of the region’s head injury victims were clarified by our study. It was observed that most of the patients (82.7%) were male, highlighting a statistically significant gender disparity in head injury occurrences. In addition, nearly half of the patients were between the ages of 21 and 40, suggesting that people in their prime are especially vulnerable to traumatic brain injuries in this region. These trends concur with the data from other regions of Saudi Arabia [5–7]. In the series by Alghamdi et al. [6], 88.3% of head injury cases in Jeddah city were males, whereas 87.3% were males in a series by Alnaami et al. [7] from the Aseer region. Although other studies indicate no gender difference [9], literature from many other parts of the world also indicates that brain injuries are more common in men [10–13].
In this study, the most frequent (n = 85; 46%) cause of head injuries was RTA, followed by falls (n = 63; 34%). This is consistent with the statistics that Saudi Arabia and most other nations have made available [5–12]. In the series by Alnaami [7], RTA accounted for 89.3% of THI in the Aseer region. Alghamdi et al. [6] found that RTA and fall from height lead to 61.4 % and 19.9% THI in Jeddah. In a series by Alkhaibary et al. [14] from Western Saudi Arabia, RTA caused THI in 57.6% followed by falls (28.3%).
The type of transportation determines the specifics of the RTA. Car accidents are common in Saudi Arabia, while motorcycle accidents are more common in studies from areas where motorbikes are popular [10–12]. Nearly 78% of all head injuries in Rwanda were caused by accidents involving motor vehicles, with pedestrians being struck by cars accounting for over 17% of these cases [12].
As is evident from the data from Saudi Arabia and elsewhere, falls from height leading to high-energy transfer are a significant causative factor for THA. Many recent studies suggest low-energy falls are also important causative factors for THI, particularly in older people. Lecky et al. [15] conducted a comparative cohort study utilizing the CENTER-TBI (Collaborative European NeuroTrauma Effectiveness Research in TBI) Registry to assess the prevalence of low-energy falls in patients reporting to the hospitals with THI and to compare their characteristics, care pathways, and outcomes to THI caused by high-energy trauma. They noted that the cases who suffer THI because of low-energy falls constitute a significant portion of the disease burden and a unique demographic group. Additionally, their results implied that energy transfer might not be a reliable indicator of intracranial damage or acute care mortality in hospitalized TBI patients and that the prehospital and emergency department THI triage in older adults may be more influenced by factors other than energy transfer level. The study suggested that it is necessary to concentrate on enhancing prevention and treatment for people who suffer traumatic brain injury from low-energy falls.
All the 185 (100%) patients in this series had undergone a non-contrast CT scan (with a bone window) as a part of the evaluation. Acute subdural hematoma (SDH), contusions/intracranial hematoma/cerebral edema, and epidural hemorrhage (EDH) were collectively detected in 118 (63.8%) and in 45 (24.3%) cases; CT scans showed an apparently normal study. Intracranial hematomas were diagnosed in 63.7% of cases in the series by Alghamdi et al. [6] based on the initial CT scan or magnetic resonance imaging (MRI) done later during admission.
In this study, 84 (45.4%) cases underwent various surgical operations, including intracranial pressure monitor insertion, evacuation of subdural/epidural hematomas, elevation of depressed skull fractures, and decompressive craniectomies, while 101 (54.6%) cases were managed conservatively. The requirement of surgical intervention had a statistically significant relation with GCS score at presentation, wherein surgical intervention was required in 81 out of 109 (74.3%) cases with GCS below 13, and only 3 out of 76 (3.9%) with GCS 14 or 15 underwent surgical operation. Similarly, the outcomes were also related to GCS score, and all the 76 (100%) cases with a GCS of 14 or 15 had favourable outcomes with no mortality or long-term disability. Among the 60 patients reporting with a GCS score of 9–13 and the 49 cases reporting with a GCS score of 8 or below, 21 (35%) and 29 (59.2%) had unfavourable outcomes, respectively, with deaths or survival with serious disabilities. These statistics concur with the data from other studies from Saudi Arabia and other regions. In the series by Alghamdi et al. [6], there were no statistically significant differences in the length of hospital stay with respect to the variables including age, gender, comorbidities, and mechanism of injury. However, the requirement of surgical intervention, the hospital stay, and the outcome were directly related to the GCS score of patients at presentation to the emergency department.
Leitgeb et al. [16] analysed the association between the GCS score at intensive care unit (ICU) discharge and the 1-year outcome of patients with THI. They retrospectively analyzed the prospectively collected observational data related to 538 patients and concluded that the GCS score at ICU discharge is a good predictor of 1-year outcome and that the patients with a GCS score <10 have a higher chance of unfavourable outcome. According to Mauritz et al. [8], who examined the outcomes of 1 172 THI patients at 3, 6, and 12 months, age, trauma severity, pupillary status, first GCS score, and CT abnormalities (such as acute SDH and a closed basal cistern on the initial CT scan) all had an impact on the long-term results. 91% of patients who had a “good recovery” were likely to stay in that group. The likelihood that a patient with “moderate disability” would make a “good recovery” was 50%. Individuals with “severe disability” had a 4% risk of dying and a 40% chance of getting better. The mortality rate was higher for those in “vegetative status” (42%) than for those who improved (31%). The first half-year following trauma was more likely to see changes than the second.
Sadaka et al. [17] performed a retrospective review of patients with THI and a GCS score of 3 and found the overall mortality of 81%. They found that 14.5% of patients with a GCS of 3 at presentation achieved a good outcome at 6 months, and 6.9% of patients with a GCS of 3 and bilateral fixed pupils on presentation achieved a good outcome at 6 months. Hence, they suggested that a GCS score of 3 on presentation in patients with THI doesn’t portend a poor prognosis for all, and there should not be any tendency to treat these patients less aggressively because of low expectations for a good outcome.
Limitations
There are several limitations in this study. Due to the retrospective design of the study, bias may have arisen from the analysis of previously archived medical data, which may have had errors or omitted information. Secondly, although our sample size of 185 patients may be representative of the region, it might not fully capture the diversity of head injury cases in larger populations. Lastly, since this article is related to the first phase of a multi-stage study related to head injuries in the Qassim region of Saudi Arabia, its scope is limited to a general overview of this healthcare issue, and it lacks the details of various traumatic disorders, and the long-term follow-up data limits to precisely evaluate the prognosis and outcomes of these individuals. These gaps are expected to be addressed as supplementary studies on the subject are released.
Notwithstanding these limitations, the current study showed that road traffic accidents and falls were the main causes of THI, underscoring the significance of taking preventive measures and suitable public health initiatives, such as traffic safety and workplace regulations, into account.
Conclusion
Traumatic head injury is a significant public health issue. The most frequent causes are traffic accidents and falls, with young individuals being the demographic most affected. Unfavourable outcomes are more likely to occur in cases of severe head injuries, as indicated by a low Glasgow coma scale. The existing situation can be improved by taking preventive action to reduce traffic accidents and workplace accidents.
Acknowledgement
The authors express gratitude to the ethics committees of Qassim University and the Ministry of Health, Qassim cluster for allowing the conduct of this study.
Contribution of authors
Both the authors have participated in data analysis and drafting of the manuscript and have approved the final manuscript.
Financial support and sponsorship
This project is entirely academic and non-commercial in nature, and it has neither sponsorship nor financial support.
Conflicts of interest
There are no conflicts of interest.
Data availability
Data can be obtained from the corresponding author upon request for a maximum of one year after the article’s publication.
Authors contributions
Sajad Ahmad Salati conceived the concept, supervised the process of obtaining the ethical committee approval to access the clinical data related to the patients, and authored the initial manuscript. Muath Ibrahim Alfallaj handled the data analysis, literature review, and editing of the manuscript. Both the authors read and approved the final manuscript. Muath Ibrahim Alfallaj and Sajad Ahmad Salati are clinicians but were not involved in the treatment or postoperative care of the patients under study.
Abbreviations
CT – Computed tomography
EDH – Epidural hematoma
GCS – Glasgow Coma Score
MRI – Magnetic resonance imaging
RTA – Road Traffic Accident
SDH – Acute subdural hematoma
THI – Traumatic head injury
References
1. Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M, Agrawal A, Adeleye AO, Shrime MG, Rubiano AM, Rosenfeld JV, Park KB. Estimating the global incidence of traumatic brain injury. J Neurosurg 2018; 130(4): 1080–1097. DOI: 10.3171/2017.10.JNS17352.
2. Herrera-Melero MC, Egea-Guerrero JJ, Vilches-Arenas A, Rincón-Ferrari MD, Flores-Cordero JM, León-Carrión J, Murillo-Cabezas F. Acute predictors for mortality after severe TBI in Spain: gender differences and clinical data. Brain Inj 2015; 29(12): 1439–1444. DOI: 10.3109/02699052.2015.1071428.
3. Iaccarino C, Carretta A, Nicolosi F, Morselli C. Epidemiology of severe traumatic brain injury. J Neurosurg Sci 2018; 62(5): 535–541. DOI: 10.23736/S0390-5616.18.04532-0.
4. Ullah S, Bin Ayaz S, Moukais IS, Qureshi AZ, Alumri T, Wani TA, Aldajani AA. Factors affecting functional outcomes of traumatic brain injury rehabilitation at a rehabilitation facility in Saudi Arabia. Neurosciences (Riyadh) 2020; 25(3): 169–175. DOI: 10.17712/nsj.2020.3.20190097.
5. Al-Habib A, A-Shail A, Alaqeel A, Zamakhshary M, Al-Bedah K, Alqunai M, Al-Enazi S. Causes and patterns of adult traumatic head injuries in Saudi Arabia: implications for injury prevention. Ann Saudi Med 2013; 33: 351–355. DOI: 10.5144/0256-4947.2013.351.
6. Alghamdi FS, Alsabbali DM, Qadi YH, Albugami SM, Lary A. Patterns and impact of traumatic brain injury at King Abdulaziz Medical City in Jeddah, Saudi Arabia: a retrospective cohort study. Cureus 2021; 13(12): e20246. DOI: 10.7759/cureus.20246.
7. Alnaami I, Alshehri S, Alghamdi S, Ogran M, Qasem A, Medawi A, Medawi A, Alshahrani S, Sarhan L. Patterns, types, and outcomes of head injury in Aseer Region, Kingdom of Saudi Arabia. Neurosci J 2019; 2019: 2782146. DOI: 10.1155/2019/2782146.
8. Mauritz W, Wilbacher I, Leitgeb J, Majdan M, Janciak I, Brazinova A, Rusnak M. One-year outcome and course of recovery after severe traumatic brain injury. Eur J Trauma Emerg Surg 2011; 37(4): 387–395. DOI: 10.1007/s00068-010-0053-6.
9. Thapa S, Baral A, Lal V, Bajracharya K, Sharma MR. Demographic and clinical profiles of patients with traumatic brain injury managed in a District Hospital in Nepal. Kathmandu Univ Med J (KUMJ) 2023; 21(84): 399–403.
10. Eshete A, Taye F. Magnitude of severe head injury and its associated factors among head injury patients in Gedeo Zone, Southern Ethiopia: a two-year retrospective study. Ethiop J Health Sci 2018; 28(3): 323–330. DOI: 10.4314/ejhs.v28i3.10.
11. Adeleye AO, Ogun MI. Clinical epidemiology of head injury from road-traffic trauma in a developing country in the current era. Front Neurol 2017; 8: 695. DOI: 10.3389/fneur.2017.00695.
12. Karim N, Mumporeze L, Nsengimana VJP, Gray A, Kearney A, Aluisio AR, Mutabazi Z, Baird J, Clancy CM, Lubetkin D, Uwitonze JE, Nyinawankusi JD, Nkeshimana M, Byiringiro JC, Levine AC. Epidemiology of patients with head injury at a Tertiary Hospital in Rwanda. West J Emerg Med 2021; 22(6): 1374–1378. DOI: 10.5811/westjem.2021.4.50961.
13. Karthigeyan M, Gupta SK, Salunke P, Dhandapani S, Wankhede LS, Kumar A, Singh A, Sahoo SK, Tripathi M, Gendle C, Singla R, Aggarwal A, Singla N, Mohanty M, Mohindra S, Chhabra R, Tewari MK, Jain K. Head injury care in a low- and middle-income country tertiary trauma center: epidemiology, systemic lacunae, and possible leads. Acta Neurochir (Wien) 2021; 163(10): 2919–2930. DOI: 10.1007/s00701-021-04908-x.
14. Alkhaibary A, Alshalawi A, Althaqafi RMM, Alghuraybi AA, Basalamah A, Shammaa AM, Altalhy AA, Abdelrahman TM. Traumatic brain injury: a perspective on the silent epidemic. Cureus 2021; 13(5): e15318. DOI: 10.7759/cureus.15318.
15. Lecky FE, Otesile O, Marincowitz C, Majdan M, Nieboer D, Lingsma HF, Maegele M, Citerio G, Stocchetti N, Steyerberg EW, Menon DK, Maas AIR; CENTER-TBI Participants and Investigators. The burden of traumatic brain injury from low-energy falls among patients from 18 countries in the CENTER-TBI Registry: a comparative cohort study. PLoS Med 2021; 18(9): e1003761. DOI: 10.1371/journal.pmed.1003761.
16. Leitgeb J, Mauritz W, Brazinova A, Majdan M, Janciak I, Wilbacher I, Rusnak M. Glasgow Coma Scale score at intensive care unit discharge predicts the 1-year outcome of patients with severe traumatic brain injury. Eur J Trauma Emerg Surg 2013; 39(3): 285–292. DOI: 10.1007/s00068-013-0269-3.
17. Sadaka F, Jadhav A, Miller M, Saifo A, O’Brien J, Trottier S. Is it possible to recover from traumatic brain injury and a Glasgow Coma scale score of 3 at Emergency Department presentation? Am J Emerg Med 2018; 36(9): 1624–1626. DOI: 10.1016/j.ajem.2018.01.051.