Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(3), pp. 205–211 DOI: https://doi.org/10.15388/LietChirur.2025.24(3).4
Aspiration and Sclerotherapy with Sodium Tetradecyl Sulfate Versus open Hydrocelectomy: An Experience with the Two Modalities of Hydrocele Management
Muhammad Munir Memon
Qassim University, Department of Surgery, College of Medicine, Saudi Arabia
E-mail: m.ghafar@qu.edu.sa
https://ror.org/01wsfe280
Sajad Ahmad Salati
Qassim University, Department of Surgery, College of Medicine, Saudi Arabia
E-mail: s.salati@qu.edu.sa
https://ror.org/01wsfe280
Mashhood Memon
SBH Health System, Bronx, New York, USA
E-mail: Mashhood.munir@gmail.com
Faiza Riaz Malik
Qassim University, Department of Surgery, College of Medicine, Saudi Arabia
E-mail: fmalik@qumc.edu.sa
https://ror.org/01wsfe280
Zaheera Saadia
Qassim University, Department of Gynecology, College of Medicine, Saudi Arabia
E-mail: zmhmod@qu.edu.sa
https://ror.org/01wsfe280
Khalid Shehzad
Qassim University, Department of Anatomy and Histology, College of Medicine, Saudi Arabia
E-mail: shhzad@qu.edu.sa
https://ror.org/01wsfe280
Abstract. Background. Hydrocele is the most prevalent cause of painless scrotal swelling. Hydrocelectomy is the gold standard of management for symptomatic hydrocele, but in recent years, aspiration and sclerotherapy have been tried as minimally invasive treatment modalities. Aim of the study. The study aims to evaluate the efficacy, safety, and cost-effectiveness of percutaneous aspiration and sclerotherapy with sodium tetradecyl sulfate (STS) compared to the standard open hydrocelectomy procedure for the treatment of symptomatic hydroceles. Methods. A retrospective analysis of the cases that were treated for symptomatic hydroceles between January 2019 and December 2023 with either open hydrocelectomy or percutaneous aspiration followed by sclerotherapy with a sodium tetradecyl sulfate-based solution was conducted. This study was undertaken after obtaining formal permission from the ethics committee. Primary outcomes included patient satisfaction and procedural success, while secondary outcomes focused on complications and the comparative costs of the procedures. Results. Thirty-seven patients were treated with aspiration and sclerotherapy, and these patients were compared with 34 patients who underwent hydrocelectomy. The mean follow-up for the aspiration and sclerotherapy group was 10.6 months, and for the hydrocelectomy group, it was 18.2 months. The patient satisfaction rate was 76% for aspiration and sclerotherapy and 90% for hydrocelectomy. The overall success rate for aspiration and sclerotherapy was 76%, compared to 86% for hydrocelectomy. The complication rate was significantly lower for aspiration and sclerotherapy (12%) compared to hydrocelectomy (29%). The cost of hydrocelectomy was almost twelve times higher than aspiration and sclerotherapy. Conclusions. Aspiration and sclerotherapy with sodium tetradecyl sulfate provide a minimally invasive, cost-effective, and safe alternative to open hydrocelectomy. Although the success rate is slightly lower than that of hydrocelectomy, its simplicity, lower complication rate, and significantly reduced cost render it a cost-effective and practical first-line approach for managing hydroceles in appropriately selected cases.
Keywords: hydrocele, hydrocelectomy, aspiration, sclerotherapy, hematoma, sodium tetradecyl sulfate.
Received: 2025-04-13. Accepted: 2025-05-12.
Copyright © 2025 Muhammad Munir Memon , Sajad Ahmad Salati, Mashhood Memon, Faiza Riaz Malik, Zaheera Saadia, Khalid Shehzad. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Hydrocele is an accumulation of serous fluid within the remnant of the processus vaginalis, resulting in scrotal enlargement [1]. It is the most prevalent cause of painless scrotal swelling, affecting 4.7% of newborns and about 1% of men above the age of 40. It can be primary or secondary as per the etiology [2], as depicted in Figure 1. Primary hydroceles are further subdivided into communicating and non-communicating depending on whether they communicate with the peritoneal cavity [3].
Communicating hydroceles are usually congenital and spontaneously resolve upon closure of the processus vaginalis by about 2 years of life. Non-communicating hydroceles result from an imbalance between secretion and reabsorption of the fluid by the tunica vaginalis and are often seen in adolescence or older age groups [4]. Secondary hydroceles are a result of trauma, malignancy, or infection.
Figure 1. Classification of hydrocele
Hydroceles are mostly asymptomatic and do not require any active treatment. However, they may progressively increase in size over time and lead to pain, interference with physical/sexual activity, infection, spermatogenic arrest, and even spontaneous rupture [5]. In symptomatic situations, open hydrocelectomy (OH) has been regarded as a gold standard of management, but it comes with issues like availability of surgeons, risks of anesthesia, pain, and surgical site complications. Although open hydrocelectomy (OH) remains the gold standard of treatment in symptomatic hydroceles, it is not without its downsides, like restricted access to trained surgeons, anaesthetic complications, postoperative pain, and wound complications. Hence, in recent years, a non-invasive treatment option in the form of aspiration of hydrocele fluid and sclerotherapy (AS) has been increasingly reported in the literature [6‒8]. A wide range of sclerosants have been reported in the literature, and there is no clear consensus on the most effective agent for hydrocele management. Sodium tetradecyl sulfate (STS) is one such sclerosing agent that has shown promising results [9]. The purpose of this study was to analyze the efficacy and complications of AS in comparison to the gold-standard treatment of OH.
Material & Methods
Study Design. Retrospective, cross sectional, descriptive study.
Data collection and analysis. The study was conducted at the Bin Tayyab Medical Complex (BTMC), Pakistan. After proper approval from the research and ethics review committee (BTMC/33/01-2025), a chart review was performed for the patients who were treated for symptomatic hydrocele by open hydrocelectomy or else percutaneous aspiration followed by sclerotherapy with an STS-based solution. The time frame selected was from January 2019 to December 2023. The data included demographics, clinical presentation, management, complications, and follow-up. Treatment was considered successful if there was no recurrence/recollection three months after the procedure. Satisfaction level was assessed by asking the patients if they were highly satisfied, satisfied, neither satisfied nor dissatisfied, dissatisfied, or highly dissatisfied with the treatment.
The exclusion criteria included the: 1) incompletely recorded data, 2) loss to follow-up, 3) application of sclerosants other than STS, 4) recurrent hydrocele, 5) infected/secondary hydrocele, 6) asymptomatic hydrocele, 7) bilateral hydrocele, 8) immunocompromised status/co-morbidities known to inhibit wound healing.
The retrieved data was analyzed with Microsoft Excel 2020 and Statistical Package for the Social Sciences (SPSS v20.0; IBMSPSS, Armonk, NY), while ensuring total anonymity of the included cases.
Technique of the procedure
Aspiration and Sclerotherapy. Percutaneous aspiration was undertaken under ultrasound guidance using a 19-G needle till fluid flowed out. This was followed by instillation of a solution containing 3% STS, 2% lidocaine hydrochloride, and 5% dextrose in normal saline. The procedure was completed in an outpatient setting. The volume of sclerosing solutions instilled was capped at 25% of the aspirated volume. Only one treatment session was conducted. Patients were followed up at 1, 3, 6, and 12 months to assess outcomes.
Hydrocelectomy. This group was operated on by standard open surgical (Jaboulay) technique wherein a median scrotal incision was made, the hydrocele was aspirated, followed by excision of excess tunica vaginalis and eversion over the spermatic cord. All the patients were hospitalized as day cases, and spinal anesthesia was usually applied.
Results
A total of 71 included cases, including the aspiration and sclerotherapy group (n = 37; 52.1%) and open hydrocelectomy (n = 34; 47.9%), were enrolled, as depicted in Table 1. The mean follow-up for the aspiration and sclerotherapy group was 10.6±2.9 months, and for the hydrocelectomy group, it was 13.2±7.2 months. Success rates for AS and OH were 76% (28/37) and 86% (30/34), respectively. Hydrocelectomy fared better in terms of success and satisfaction rates (Table 2, 3), but in terms of complication rate (Figure 2), AS was superior (12% vs. 29%; p-value < 0.005).
Table 1. Patient demographics and hydrocele characteristics
|
Group |
Aspiration & Sclerotherapy |
Open Hydrocelectomy |
|
(n = 37) |
(n = 34) |
|
|
Mean age (years) |
64.6±٢٣.١ |
55.2±١٤.٤ |
|
Side of hydrocele |
17 left, 20 right |
15 left, 19 right |
|
Mean hydrocele volume (ml) |
260 |
N/A |
Table 2. Primary outcomes: success & satisfaction rates
|
Group |
Success rate |
Satisfaction rate |
||||
|
Highly |
Satisfied |
Neutral |
Dissatisfied |
Highly |
||
|
Aspiration & Sclerotherapy |
76% (28/37) |
27% (10/37) |
49% (18/37) |
13% (5/37) |
11% (4/37) |
0% (0/37) |
|
Open Hydrocelectomy |
86% (30/34) |
47% (16/34) |
41% (14/34) |
9% (3/34) |
3% (1/34) |
0% (0/34) |
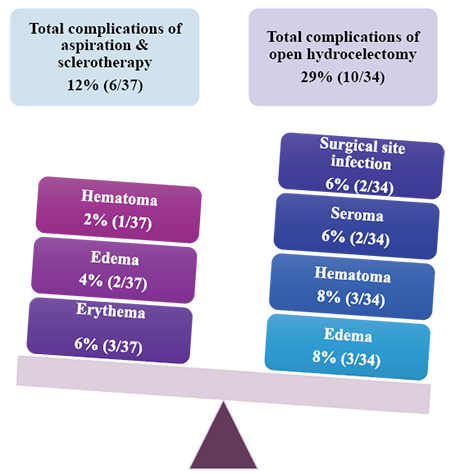
Figure 2. Secondary outcomes ‒ complications of hydrocele management modalities
Table 3. Secondary outcomes ‒ complications of hydrocele management modalities
|
Cost Comparison |
|
|
Procedure |
Cost per procedure |
|
Aspiration and Sclerotherapy |
PKR 2 400.00 |
|
Open Hydrocelectomy |
PKR 29 000.00 |
Discussion
Aspiration and sclerotherapy (AS) have been reported as an alternative management option to hydrocelectomy for hydrocele, and they offer the advantage of being a simple, outpatient-based procedure with significantly shortened recovery time and reduced costs [10]. A variety of sclerosants have been used with varying levels of efficacy for the treatment of hydroceles, including polidocanol, phenol, sodium tetradecylsulfate (STS), tetracycline, doxycycline, and alcohol, though there is still a lack of consensus on the most effective agent. STS functions by causing endothelial cell damage and inducing an inflammatory response that causes fibrosis, thereby reducing the ability of fluid secretion. In our study, a success rate of 76% (28/37) was attained with 3% STS. This rate is comparable to the results attained by Khaniya et al. [8] and Musa et al. [9] after a single treatment session with a similar concentration of STS.
The success rate of AH is lower than that achieved in this study by OH. The patient satisfaction level (highly satisfied or satisfied) was also higher in OH, and that can be attributed to the difference in success rates. These results concur with the current literature, as multiple studies [8, 11] have highlighted the need for multiple treatment sessions of AS to reach the similar curative outcomes as OH.
In terms of secondary outcomes, the AS was more advantageous than OH. The complication rate of AS in our study was 12%, which concurs with literature, where the complication rate ranges from 8% to 10%. Self-resolving erythema was the most common complication, occurring in 3 (6%) of cases. Musa et al. [9] have reported post-procedural erythema in 43.9% of patients, which had resolved within 1 week. Hydrocelectomy had a wider range of complications, including postoperative edema, surgical site infection, and collection of hematoma/seroma.
Korkes et al. [12] in 2021 evaluated the outcomes and costs associated with surgery versus sclerotherapy as treatment of hydroceles. They enrolled 39 cases who had undergone hydrocelectomy by the Jaboulay technique and 14 cases of a similar age group who had undergone sclerotherapy. Success rates were 94.8% and 92.8% after surgery and sclerotherapy, respectively. The mean cost per patient was US$2,558.69 in the Surgery Group and US$463.58 in the Sclerotherapy Group (p < 0.0001), representing an economy of 81% for patients managed by sclerotherapy. Surgical management was 5.5-fold more expensive than sclerotherapy. In our study, the cost for OH was calculated to be about 12-fold as compared to AS (p < 0.005). Hence, AS can be particularly important in economically underdeveloped countries where access to healthcare resources may be limited. Furthermore, since OH poses higher risks, AS may not be a suitable option for patients with multiple comorbidities or advanced age [13, 14].
Even though uncommon, complications have been reported after sclerotherapy, and an important concern in the young patients is the impact on spermatogenesis. Shan et al. [15] addressed this issue and evaluated the effects of sclerotherapy with alcohol. Post-sclerotherapy spermograms displayed a reduction in concentration, motility, and sperm morphology up to 6 months post-procedure, with a return to normalcy at 12 months after the procedure. They concluded that sclerotherapy may be performed safely in young men who wish to have fertility.
Limitations
An important limitation of this study is a smaller sample size, making it difficult to generalize the outcomes to the larger population. Another limitation is that the study is retrospective in nature and hence relies on the data that is pre-recorded without following any study protocols, leading to exclusions due to incompleteness.
Conclusions
Aspiration and sclerotherapy using sodium tetradecyl sulfate provide a viable, minimally invasive option for the treatment of hydrocele. This approach offers a cost-effective alternative to hydrocelectomy and may be appropriate as an initial management strategy for selected patients. However, hydrocelectomy remains the definitive treatment for patients seeking higher success rates and long-term resolution.
Abbreviations
AS ‒ Aspiration and Sclerotherapy,
OH – Open Hydrocelectomy,
SPSS ‒ Statistical Package for the Social Sciences,
STS ‒ Sodium Tetradecyl Sulfate.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Financial acknowledgements
The author(s) received no financial support for the authorship, research, or publication of this article.
Contribution of the authors
MMM conceived the concept, supervised the process of obtaining the ethical committee approval to access clinical data related to the patients, and obtained the data. MM and SAS drafted the initial manuscript. Other authors handled data analysis, literature review, and editing of the manuscript. All the authors read and approved the final manuscript. MIA and SAS are clinicians but were not involved in the treatment or postoperative care of the patients under study.
Data availability
Data would be retained safely and be made available on request, by the corresponding author for a year after the date of publication.
References
1. Wampler SM, Llanes M. Common scrotal and testicular problems. Prim Care 2010; 37(3): 613‒626. DOI: 10.1016/j.pop.2010.04.009.
2. Dagur G, Gandhi J, Suh Y, Weissbart S, Sheynkin YR, Smith NL, Joshi G, Khan SA. Classifying hydroceles of the pelvis and groin: an overview of etiology, secondary complications, evaluation, and management. Curr Urol 2017; 10(1): 1‒14. DOI: 10.1159/000447145.
3. Hoang VT, Van HA, Hoang TH. Updated classification system for primary hydrocele. Abdom Radiol 2022; 48(1): 387‒389. DOI: 10.1007/s00261-022-03697-w.
4. Basaif WS, Murshid AK, Alhadi YM, Albarman SD, Almunaikh MJ, Alsaffar AM, Aljohani AS, Alshehri AA, Aloufi KS, Alnami AA, Asiri AA, Siyam ZH. Prognosis and management of communicating and non-communicating hydrocele. J Pharm Res Int 2021; 33: 347‒353. DOI: 10.9734/jpri/2021/v33i43b32562.
5. Flores VX, Wallen JJ, Martinez DR, Carrion R. Deflate-gate: conservative management of a large ruptured hydrocele. Urol Case Rep 2015; 3(6): 198‒200. DOI: 10.1016/j.eucr.2015.08.002.
6. Francis JJ, Levine LA. Aspiration and sclerotherapy: a nonsurgical treatment option for hydroceles. J Urol 2013; 189(5): 1725‒1729. DOI: 10.1016/j.juro.2012.11.008.
7. Beiko DT, Kim D, Morales A. Aspiration and sclerotherapy versus hydrocelectomy for treatment of hydroceles. Urology 2003; 61(4): 708‒712. DOI: 10.1016/s0090-4295(02)02430-5.
8. Khaniya S, Agrawal CS, Koirala R, Regmi R, Adhikary S. Comparison of aspiration-sclerotherapy with hydrocelectomy in the management of hydrocele: a prospective randomized study. Int J Surg 2009; 7(4): 392‒395. DOI: 10.1016/j.ijsu.2009.07.002.
9. Musa O, Roy A, Ansari NA, Sharan J. Evaluation of the role of sodium tetradecyl sulfate as a sclerosant in the treatment of primary hydrocele. Indian J Surg 2015; 77(S2): 432‒437. DOI: 10.1007/s12262-013-0866-8.
10. Campbell BR, Bingham R. Hydrocele management: a review of current techniques and outcomes. World J Urol 2021; 39(7): 2309‒2317. DOI: 0.1007/s00345-020-03321-3.
11. Shan CJ, Lucon AM, Arap S. Comparative study of sclerotherapy with phenol and surgical treatment for hydrocele. J Urol 2003; 169(3): 1056‒1059. DOI: 10.1097/01.ju.0000052680.03705.40.
12. Korkes F, Teles SB, Nascimento MP, Almeida SS, Codeço AM. Comparison of outcomes and costs of surgery versus sclerotherapy to treat hydrocele. Einstein (Sao Paulo) 2021; 19: eGS5920. DOI: 10.31744/einstein_journal/2021GS5920.
13. Shakiba B, Heidari K, Afshar K, Faegh A, Salehi-Pourmehr H. Aspiration and sclerotherapy versus hydrocelectomy for treating hydroceles: a systematic review and meta-analyses. Surg Endosc 2023; 37(7): 5045‒5051. DOI: 10.1007/s00464-023-10143-5.
14. Taylor WSJ, Cobley J, Mahmalji W. Is aspiration and sclerotherapy treatment for hydroceles in the aging male an evidence based treatment? Aging Male 2019; 22(3): 163‒168. DOI: 10.1080/13685538.2018.1425987.
15. Shan CJ, Lucon AM, Pagani R, Srougi M. Sclerotherapy of hydroceles and spermatoceles with alcohol: results and effects on the semen analysis. Int Braz J Urol 2011; 37(3): 307‒312; discussion 312‒333. DOI: 10.1590/s1677-55382011000300003.