Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(4), pp. 325–329 DOI: https://doi.org/10.15388/LietChirur.2025.24(4).10
Surgical Challenges in Severe Fixed Extension Deformity of the Right Knee Post Multiple Sclerotherapy for Arterio-Venous Malformation: A Case Report
Vipin V. Nair
Plastic Reconstructive Surgeon, AFMC, Pune, India
E-mail: vipinvenugopalnair@gmail.com
Chetan Sood
HOD Dept of Orthopaedics, AFMC, Pune, India
E-mail: drchetansood@gmail.com
Abstract. Introduction. Acquired arteriovenous malformations (AVMs) often result from minor trauma. AVMs exhibit diverse clinical manifestations and an unpredictable clinical course. This document addresses the management challenges associated with restoring mobility in a patient who experienced severe extension lock of the right knee following repeated sclerotherapy for an extensive arteriovenous malformation of the right vastus lateralis muscle. Main symptoms and important clinical findings. The patient sustained a contusion of the right thigh after a trivial trauma, subsequently developing an extensive arteriovenous malformation in the right vastus lateralis over several years. The patient underwent multiple sclerotherapy sessions with 10% polidocanol for AVM control over one year. Gradually, the patient’s right knee became locked in extension, resulting in functional disability. The main diagnoses, therapeutic interventions, and outcomes. Clinical examination revealed a 10x8 cm stony hard swelling in the lateral aspect of the right thigh. MRI indicated a low-flow venous malformation involving the right vastus lateralis with atrophy of the proximal portion. A CT-angiogram identified a feeder from the medial circumflex femoral artery. The patient underwent surgical exploration and excision of the sclerosed vastus lateralis and part of the vastus intermedius muscle, with a Tensor Fascia Lata graft applied to the exposed femoral bone surface. The patient recovered well, achieving an active knee flexion of 110 degrees, and is now able to sit and drive comfortably. Conclusion. The treatment of AVMs presents significant challenges. Minimally invasive methods are foundational to management but can lead to severe soft tissue fibrosis and functional disability. Surgery becomes necessary in complicated cases and for managing complications arising from minimally invasive procedures. Optimal outcomes require individualized multi-departmental management for all patients.
Keywords: arterio-venous malformation, sclerotherapy, knee joint
Received: 2025-07-04. Accepted: 2025-09-01.
Copyright © 2025 Vipin V. Nair, Chetan Sood. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Arteriovenous malformations (AVMs) exhibit various clinical presentations and an unpredictable clinical course. They can be associated with serious conditions such as active haemorrhage, high output heart failure, and ischemic necrosis due to the “steal” phenomenon [1, 2]. AVM expands because of the high blood flow between the arteries and veins. Factors like trauma, hormonal changes, or incomplete treatment of an AVM with a remnant nidus can contribute to the rapid growth of the AVM [3, 4]. We discuss the challenge of restoring mobility in a patient with severe right knee extension lock following multiple sclerotherapies for extensive AVM of the right vastus lateralis muscle.
Case report
A 50-year-old male with no known comorbidities presented with a history of stiffness in the right knee joint for the last seven years. Ten years earlier, he experienced a minor fall from his two-wheeler, resulting in a contusion injury to the lateral aspect of his right thigh. Subsequently, he developed an extensive arteriovenous malformation (AVM) in the right vastus muscle. Multiple sessions of injection sclerotherapy with 10% Polidocanol were administered to reduce the progression of the AVM by an interventional radiologist over the next year. Gradually, his right knee became locked in extension. He was functionally disabled as he was not able to sit normally and had difficulty driving and riding vehicles.
On examination, his knee was locked in extension with no range of motion. There was a 10×8 cm stony hard swelling over the lateral aspect of the right thigh. His haematological and biochemical profiles were normal. A contrast-enhanced MRI was carried out which showed diffuse hyperintensities involving the lateral compartment of the right thigh within the vastus lateralis muscle. The vertical extent of the abnormal areas was 26 cm (CC) and measured 8.4 (AP)×4.2 cm (TR). Multiple intramuscular venous channels were noted within the abnormal area. The MR angiogram showed two feeding branches arising from the right mid-Superficial Femoral Artery coursing towards the abnormal area within the vastus lateralis muscle. There was evidence of cortical thickening in the underlying shaft of the right femur along its lateral aspect, most likely reactive. There was mild atrophy of proximal muscles of the right thigh. A contrast enhanced Angiogram revealed a feeder from the medial circumflex femoral artery. A hypodense lesion with relatively ill-defined margins measuring 26×5.4×7.9 cm (CC×TR×AP) was seen in the right thigh in the intramuscular plane involving the vastus lateralis muscle. It showed calcified phleboliths on plain study. The angiography study also showed nodular enhancement with two dominant arterial branches from the middle one-third of the superficial femoral artery, the largest measuring 3.5 mm in maximum diameter. Multiple small arterial feeders were also seen from branches of the profunda femoris artery. On venous phase and delayed study, multiple venous draining channels were seen in the superficial and deep femoral vein.
The patient underwent exploration and excision of the sclerosed vastus lateralis and part of the vastus intermedius muscle. The excision resulted in a large raw area over the femur and a cavity after closure of the skin. The raw area of the femur was covered with a tensor fascia graft measuring 20×8 cm harvested from the same thigh. The fascia graft was fixed, and the knee was mobilised to 130 degrees intraoperatively before wound closure with closed suction drain. The drain was removed after 8 days when the output was not significant. He was placed on a continuous passive motion machine for the next ten days and recovered well, achieving a knee active flexion of 60 degrees and discharged home after 14 days with advice on continuing limb passive mobiliser in home (Figure 1).
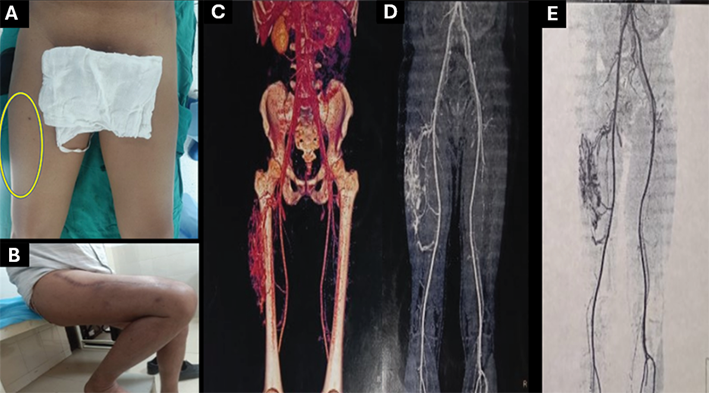
Figure 1. (A) Pre operative and (B) post operative clinical picture of the right thigh. C, D, E. MR Angio and MRI images of the right thigh showing the extend of AVM and the feeding vessels.
Follow-up
Four weeks post-surgery, the patient presented with a significant seroma collection in the thigh cavity following the removal of the vastus muscle. The primary concern was the potential for flap failure, which could result in muscle adherence and subsequent stiffness. The seroma was aspirated on alternate days under ultrasound guidance for next 10 days. This settled the problem without requirement for reexploration. After six weeks, the right knee mobilisation under anaesthesia was performed again. He recovered well with 110 degrees of active knee flexion and can sit comfortably and drive his car (Figure 2).
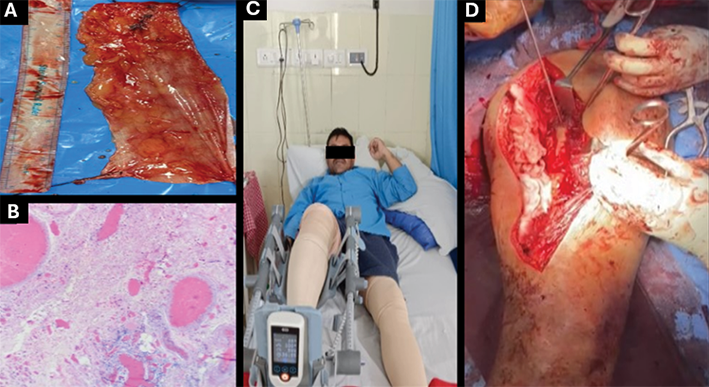
Figure 2. A. Tensor Fascia Lata harvested. B. HPE of the lesion showing muscles interlaced with abundant endothelial lined channels. C. Usage of Continuous Passive Mobilizer. D. Application of Tensor Fascia Flap over resultant raw surface following excision of the vastus lateralis muscle of right thigh.
Discussion
AVMs are rare congenital vascular anomalies characterized by early quiescence, late expansion, and eventual infiltration and destruction of local soft tissue and bone. The extremities frequently exhibit these lesions. Bony involvement in AVMs has been reported to occur in up to 31% of cases. The Bernese Congenital Vascular Malformation Registry prospectively enrolled 506 patients, 31 (6%) with AVM. Simple AVM was found in 22 (71%) and combined or syndromic AVM with limb overgrowth in 9 (29%). Common symptoms included pain (25; 81%), swelling (21; 68%), and soft tissue hypertrophy (13; 42%). Syndromic patients had higher rates of bleeding (67% vs. 5%; p < 0.001), malformation-related infection (44% vs. 5%; p = 0.017), and leg length difference (56% vs. 14%; p = 0.049) [5].
Surgical resection of AVMs presents significant challenges, and recurrence is common if resection is incomplete [6]. Consequently, it is imperative that only surgically resectable lesions are chosen for surgical intervention, whether performed alone or in conjunction with embolo-sclerotherapy techniques applied preoperatively or postoperatively. Preoperative embolization may be beneficial prior to surgical intervention due to the heightened risk of massive bleeding associated with these anomalies. Complete eradication of the nidus of an AVM is recognized as the only potential cure. Management of post operative complications listed above and physiotherapy for functional rehabilitation is important following surgical management [7].
Conclusion
Arteriovenous malformations (AVM) are difficult to treat. Management is mostly done with minimally invasive techniques, but complex cases and complications require surgery. All patients need individualised, multi-departmental care for best results. Aggressive blood flow control reduces surgical complications and may cure. Early detection and management of AVMs reduce morbidity and should be tailored to their size, type, and anatomical location.
Author contribution
Dr. Vipin V. Nair ‒ conceptualization, methodology, formal analysis, investigation, writing ‒ original draft, writing ‒ review and editing.
Dr. Chetan Sood ‒ visualization, conceptualization, methodology, formal analysis, investigation, writing ‒ original draft, writing ‒ review and editing.
Statement of Ethics. Subject have given his written informed consent to publish his case including publication of images.
Study approval statement. The study has been granted an exemption from requiring ethical approval.
Conflict of interest. No conflict of interest.
Funding sources. Non funded.
References
1. Lee YO, Hong SW. Treatment of large arteriovenous malformation in right lower limb. Korean J Thorac Cardiovasc Surg 2014; 47(1): 66‒70. DOI: 10.5090/kjtcs.2014.47.1.66.
2. Hou F, Chen J, Xia M, Ding K, Zeng Q, Liu W. Percutaneous sclerotherapy with polidocanol under the guidance of ultrasound for venous malformations in children ‒ a retrospective cohort study from a single tertiary medical center. Medicine (Baltimore) 2020; 99(9): e18839. DOI: 10.1097/MD.0000000000018839.
3. Bernhard SM, Tuleja A, Laine JE, Haupt F, Häberli D, Hügel U, Rössler J, Schindewolf M, Baumgartner I. Clinical presentation of simple and combined or syndromic arteriovenous malformations. J Vasc Surg Venous Lymphat Disord 2022; 10(3): 705‒712. DOI: 10.1016/j.jvsv.2021.10.002.
4. Lim CS, Evans N, Kaur I, Papadopoulou A, Khalifa M, Tsui J, Hamilton G, Brookes J. Incidence of major complication following embolo-sclerotherapy for upper and lower extremity vascular malformations. Vascular 2021; 29(1): 69‒77. DOI: 10.1177/1708538120937616.
5. Zobel MJ, Moses W, Walther A, Nowicki D, Howell L, Miller J, Zeinati C, Anselmo DM. Management challenges of a large upper extremity vascular malformation in a patient with capillary malformation-arteriovenous malformation syndrome. J Vasc Surg Venous Lymphat Disord 2021; 9(3): 781‒784. DOI: 10.1016/j.jvsv.2020.07.001.
6. Bota N, Ignat P, Avram J, Ivan V, Bota L. Indicaţiile tratamentului chirurgical în malformaţiile venoase ale membrelor inferioare [The indications for surgical treatment in venous malformations of the lower extremities]. Chirurgia (Bucur) 1994; 43(1): 32‒37.
7. Zhang Y, Liang Z, Lv Z, Lu Q, Wu M, Li L, Cao L, Liu J, Cui J. A multicenter retrospective analysis of the clinical outcome following endovascular treatment of extremity arteriovenous malformation. Int Angiol 2023; 42(3): 260‒267. DOI: 10.23736/S0392-9590.23.04978-7.