Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(4), pp. 274–283 DOI: https://doi.org/10.15388/LietChirur.2025.24(4).3
Cylindroma of the Breast: A Systematic Review of a Rare Disorder
Sajad Ahmad Salati
Qassim University, Department of Surgery, College of Medicine, Kingdom of Saudi Arabia
E-mail: s.salati@qu.edu.sa
https://orcid.org/0000-0003-2998-7542
https://ror.org/01wsfe280
Saleh Alsuwaydani
Qassim University, Department of Surgery, College of Medicine, Kingdom of Saudi Arabia
E-mail: s.alsuwaydani@qu.edu.sa
https://orcid.org/0000-0003-0817-3929
https://ror.org/01wsfe280
Abstract. Introduction. Cylindroma of the breast is a rare disorder, and only a few cases have been reported in the literature. Due to its rarity, this article was drafted to study the cases published over the last decade and thereby try to explain the current patterns in clinical presentation, diagnosis, treatment, and outcomes. Methods. A systematic literature search was conducted through electronic databases applying the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Results. There were 9 case reports with 10 female patients, ranging in age from 55 to 80 years. Local excision was the most common modality of treatment. The outcome was excellent with no recurrence. Conclusion. Cylindroma of the breast is rare with an excellent prognosis. It needs to be kept in mind as a differential diagnosis of triple-negative breast tumours or the solid basaloid variant of adenoid cystic carcinoma to avoid unnecessary overtreatment with associated morbidity.
Keywords: cylindroma, breast neoplasm, adenoid cystic carcinoma, jigsaw pattern, dermal analogue tumour, breast adnexal tumour, triple negative phenotype, systematic review.
Received: 2025-05-14. Accepted: 2025-07-01.
Copyright © 2025 Sajad Ahmad Salati, Saleh Alsuwaydani. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Cylindroma is a benign neoplasm of the skin appendages. The word “cylindroma” was first coined by Billroth in the year 1959, as the histopathological appearance of cells resembles a cylinder in cross section [1].
They most often occur in the scalp [2] and face and neck regions [3], though uncommonly, they may be encountered in salivary glands, lungs, and kidneys [4]. Cylindroma of the breast (CB), arising within its parenchyma, is an extremely rare entity. It is usually present as a solitary lesion or may exist in association with other lesions. Only a few isolated cases have been reported in the peer-reviewed literature since its first documentation by Gokaslan et al. [5] in 2001. Due to the rarity, there are no articles that might give an institutional experience comprising a larger number of cases, and hence, this article was drafted to systematically analyse the cases reported in the peer-reviewed literature over the last decade and thereby try to identify patterns in clinical presentation, diagnosis, treatment, and outcomes.
Materials and methods
Methods. A systematic literature search was conducted through electronic databases and academic blogs, including PubMed, ResearchGate, PsycINFO, Scopus, and Google Scholar, using the key words and terms “breast cylindroma”, “benign breast lump”, and “rare breast neoplasm”. The search was carried out by using individual keywords with a combination of Boolean logic (AND). Only English literature was considered for inclusion in this study. The time frame fixed was 2016–2025.
Criteria for considering studies. Articles, including case series and case reports, were published during the selected time frame and provided an account of the variables that were included in the review process.
Participants and outcome measures. Only those cases in which the diagnosis of cylindroma of the breast (CB) had been confirmed by histopathological/molecular analysis were included.
The variables (Table 1) analyzed include: [i] age of the patient; [ii] gender; [iii] clinical presentation; [iv] findings on imaging; [v] management; [vi] operative findings; [vii] histopathology; [viii] immunochemistry; and [ix] postoperative course.
Exclusion. The articles that did not provide detailed information about the variables under study, were excluded. Furthermore, the publications from non-English literature were also excluded.
Methodological quality checking. Checklist items from Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) and previously published peer-reviewed literature were used for comparison with the checklist that was drafted for this study.
Data Synthesis (extraction and analysis). Data related to the variables was extracted and arranged in form of Tables 1 & 2. The collected data was then analysed with Microsoft Excel (Office Version 16). The information was presented using frequencies, summary measures, tables, and figures as shown in the results. P < 0.05 and 95% confidence level were used as a difference of statistical significance.
Results
Study selection. As seen in Figure 1, the electronic database search yielded a total of 27 publications. Twelve duplicate articles were eliminated and then titles and abstracts of 15 articles were screened. This allowed for the retrieval of 14 possibly relevant articles for the qualifying requirements. After further exclusion of 5 articles due to unavailability or deficiency of data related to the variables under study or the lack of relationship with the disorder under study, the review ultimately analysed a total of 9 case reports.
Study characteristics. Study characteristics are presented in Tables 1 and 2.
Table 1. Patient characteristics (demographics and imaging studies)
|
S No. |
Series / Year |
Age (years) / |
Clinical |
PH/FH/Co |
Imaging studies |
|||
|---|---|---|---|---|---|---|---|---|
|
Mammography |
Ultrasound |
MRI |
CT scan |
|||||
|
1. |
Papaoikonomou |
62/F |
Asymptomatic and detected on SM. |
Unremarkable. |
7.5 mm nodule with well-defined borders of the lower outer quadrant of the left breast, next to the areola. |
7.5×5 mm hypoechoic lesion at the four o’clock position of the left breast (BI-RADS 2); during F/U, size increased to 11.6×6 mm. |
Nodule with lobulated borders, type 2 enhancement and BI-RADS 4 category. |
‒ |
|
2. |
McGhee |
71/F |
Incidentally detected pea-shaped palpable lump. |
Previously treated two cancers: 1) SCC of the nasal root; 2) anal SCC. |
An oval mass in the lower inner quadrant in the left breast. |
Anechoic, circumscribed, posterior acoustic enhancement, no internal vascularity, adjacent to skin, about 7 mm, at 8 o’clock, 12 cm from the nipple. |
MRI (performed 8 years ago): a circumscribed oval homogeneously enhancing T2-hyperintense mass. |
‒ |
|
3. |
Steinwehr |
79/F |
Asymptomatic, detected while evaluation for chest trauma. |
FH: daughter had BC. Co: HT, MO. |
‒ |
‒ |
‒ |
15 mm nodular asymmetric soft tissue density in the left breast upper inner quadrant. |
|
4. |
Escher-Michlig |
60/F |
Asymptomatic, detected during SM. |
Invasive carcinoma (NST) in right breast 9 years earlier; histiocytoma of the skin. |
A 5 mm nodule in within the left breast. |
‒ |
‒ |
‒ |
|
5. |
Liu |
80/F |
Asymptomatic, incidentally detected right breast lump. |
Hypertension. |
‒ |
4.04 cm x 2.08 cm right breast lump, BI-RADS ٤‒5. Few axillary nodes. |
‒ |
‒ |
|
6. |
Halima |
71/F |
Slowly enlarging right breast lump – 5 years. |
Previously treated renal cancer, colonic cancer and BCC skin. |
A 25 mm, well-circumscribed nodule within the right breast located at 12 o’clock. |
‒ |
‒ |
‒ |
|
7. |
Ahmed |
63/F |
Painless slowly enlarging right breast lump of 5 years duration. |
Nothing significant. |
A well-circumscribed mass with no micro calcifications, skin or nipple changes. |
A lobulated hypoechoic mass with a micro lobulated margin with increase heterogeneity but no increase vascularity |
‒ |
‒ |
|
Ahmed |
58/F |
Painless, slowly growing left breast mass – many months. |
Nothing significant. |
A well-circumscribed mass in the left breast with no micro calcifications nor skin or nipple changes. |
A lobulated hypoechoic mass with a micro-lobulated margin and no increase vascularity or surrounding invasion (BI-RADS 3). |
‒ |
‒ |
|
|
8. |
Patel |
55/F |
Asymptomatic left breast lump detected on screening mammography. |
Bilateral sub-glandular saline breast implants; strong maternal family history of cancers; genetic screening had revealed a PMS2 gene mutation, which is linked to Lynch syndrome. |
A lobulated mass in the upper inner quadrant adjacent to the silicon implant. |
A 0.8 cm lobulated hypoechoic mass in the left upper inner quadrant with irregular borders and increased vascularity, closely adherent to the implant capsule. |
‒ |
‒ |
|
9. |
Fusco et al. / 2016 [14] |
66/F |
Asymptomatic left breast lump detected on screening mammography. PE: nothing significant. |
Nothing significant. |
An irregular dense shadow involving a wide area of the upper outer quadrant of the right breast in the background of increased parenchymal density. |
A suspicious hypoechoic lesion measuring 0.9 cm, about 6 cm away from the nipple. |
‒ |
‒ |
SCC ‒ squamous cell carcinoma, BC ‒ breast cancer, SM ‒ screening mammography, F/U ‒ follow-up, BI-RADS ‒ Breast Imaging Reporting and Data System, PE ‒ physical examination, Co ‒ comorbidities, HT ‒ hypertension, MO ‒ morbid obesity, NST ‒ no special type, BCC ‒ basal cell carcinoma, LAD ‒ lymphadenopathy.
Table 2. Patient characteristics (histopathology, immunochemistry and management)
|
S No. |
Series |
Management |
Histopathology |
Immunochemistry |
Postoperative phase |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
|
CD7 |
P 63 |
ER |
PR |
Her2 |
Others |
|||||
|
1. |
Papaoikonomou et al. [6] |
Wide excision. |
A 9 mm tumour within the breast tissue, not attached to the overlying skin, consisting of inner epithelial and outer myoepithelial cells in tightly packed cell islands forming the typical mosaic/jigsaw pattern. |
P |
P |
N |
N |
N |
‒ |
Uneventful; no recurrence at 6 months. |
|
2. |
McGhee |
Wide local excision. |
Islands of epithelial cells composed of peripheral basaloid cells and central larger cells with oval vesicular nuclei, surrounded by thickened membrane material with hyalin globules. |
‒ |
P |
N |
‒ |
‒ |
CK5/6: P; |
Uneventful. |
|
3. |
Steinwehr |
Lumpectomy, axillary SLND. |
A 24 mm biphasic neoplasm composed of densely packed, basaloid tumor islands surrounded by compact, eosinophilic basement membrane ‒ like material, arranged in a “jigsaw” pattern. |
‒ |
P |
P |
N |
N |
GATA3: P |
Uneventful. |
|
4. |
Escher-Michlig |
Wide local excision. |
A non-encapsulated tumor composed of cell nests of dual population of cells and arranged in a distinct “jigsaw” pattern. |
‒ |
‒ |
N |
N |
N |
‒ |
Uneventful, no recurrence at 2 years. |
|
5. |
Liu |
Radical mastectomy. |
Islands of epithelial cells surrounded by dense membrane materials; hyaline globules in many cell islands; in some areas, cells arranged in cords, occasional mitosis. |
‒ |
‒ |
N |
N |
‒ |
S100: P; TP63: P; |
Uneventful, no recurrence at 2 years. |
|
6. |
Halima |
Wide local excision. |
A 25 mm non-capsulated tumor composed of nests of basaloid cells arranged in a “jigsaw” pattern; some nests morphologically biphenotypic with tendency for whorling. |
‒ |
P |
N |
N |
N |
Mg: P; GATA3: P, |
Uneventful. |
|
7. |
Ahmed |
Wide local excision. |
Gross examination: a firm tumour with 1.6 cm maximum dimension. Microscopic exam: irregularly shaped islands and nests of cells with a characteristic “jig-saw” or “mosaic” appearance enclosed by thin strand of eosinophilic stroma; the cells at the centres of the cord were closely packed with scanty cytoplasm and large vesicular nuclei. At the periphery, the cells had elongated, basophilic nuclei; no evidence of atypia nor mitosis or necrosis seen. |
‒ |
‒ |
N |
N |
‒ |
GCDFP-15: P; |
Uneventful. |
|
Excision biopsy. |
Gross examination: firm mass measuring 1.8x2.2x1.2 cm. Microscopic exam: like the above case. |
‒ |
‒ |
N |
N |
‒ |
‒ |
Uneventful. |
||
|
8. |
Patel et al. |
Excisional biopsy followed by re-excision. |
A low-grade basaloid tumour of uncertain malignant potential with an involved margin, consistent with but not definitively, a cylindroma. |
‒ |
P |
N |
N |
N |
‒ |
Uneventful. |
|
9. |
Fusco et al. |
Quadrantectomy with sentinel lymph node excision. |
Restudy of the core biopsy and the excision specimen revealed a non-encapsulated but relatively well demarcated lesion with irregular borders composed of nests and trabeculae of tumor cells arranged in a jigsaw puzzle pattern; no nuclear atypia or mitosis. |
‒ |
‒ |
N |
N |
N |
RT-PCR, FISH |
Uneventful, alive without recurrence at 3 years. |
Mg ‒ mammaglobin, SLND ‒ sentinel lymph node dissection, HWP ‒ hook wire placement, NL ‒ needle localization.

Figure 1. Flowchart of the reviewed articles
There were 9 case reports with 10 patients. All (n = 10; 100%) of them were female, ranging in age from 55 to 80 years (mean 66.6±8.55 years). The clinical presentation was painless breast lump with no skin or nipple changes as shown in Table 3.
Table 3. Clinical presentation of patients of cylindroma of breast
|
Clinical presentation |
Number (presentation) |
|
Asymptomatic, detected on screening mammography |
4 (40%) |
|
Asymptomatic, detected on evaluation for chest trauma |
1 (10%) |
|
Incidentally self-detected painless lump |
2 (20%) |
|
Slowly growing painless lump over months to years |
3 (30%) |
|
Total |
10 (100%) |
In half of the cases, there was a history of cancer, either in self (n = 3; 30%) or in the family (n = 2; 20%). The cancers were solitary or multiple cutaneous in nature (n = 2; 20%). One patient had bilateral sub-glandular saline breast implants, strong maternal family history of cancers and genetic screening had revealed a PMS2 gene mutation, which is linked to Lynch syndrome.
Mammography and breast ultrasonography were undertaken in 8 (80%) and 7 (70%) patients respectively. Additionally, MRI breast in 2 (20%) and CT scan in 1 (10%) case were undertaken. BI-RADS (Breast Imaging Reporting and Data System) scoring was documented in 5 (50%) cases; the scores were 4 (n = 2; 20%), 3 (n = 2; 20%) and 2 (n = 1; 10%). The management options adopted are as depicted in Figure 2, with wide local excision being the most common option (n = 5; 50%).
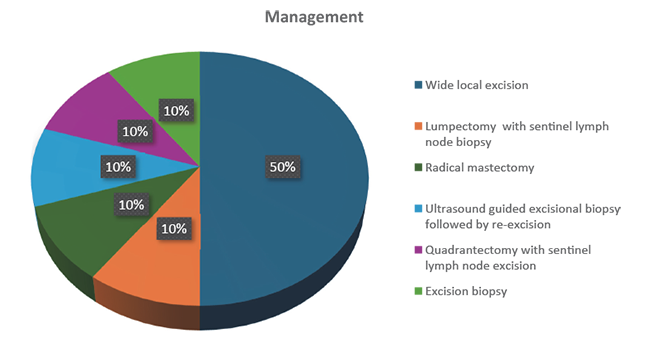
Figure 2. Management options adopted for cylindroma of breast
Histopathological analysis confirmed the diagnosis, and the general pattern was of a non-encapsulated tumour present within normal breast parenchyma and no had direct connection with the overlying skin and composed of cell nests of dual population of cells and arranged in a distinct “jigsaw” pattern. Atypia and mitosis were absent in 9 (90%) cases and only in 1 (10%), very occasional mitosis were reported. Estrogen receptors (ER) were tested in all cases and were negative in 9 (90%); progesterone receptors (PR) were tested in 9 cases and were negative in all. P63 was tested in 5 cases and was positive in all. Triple negative status (ER, PR, Her2 negative) was documented in 5 (50%) cases. Postoperative phase was uneventful in all (100%) and there was no recurrence over the follow-up period varying from 6 months to 3 years.
Discussion
Cylindroma of the breast (CB) is a rare benign disorder, and after its first documentation by Gokaslan et al. [5] in 2001, only a few case reports have been published. This article is the first attempt to assemble the data from the last decade to create a broader image about the disorder with respect to clinical presentation, imaging, treatment, and outcomes.
CB is detected incidentally by breast cancer screening modalities or else by self-detection of lumps. CB appears to be the disorder manifesting as solitary lumps, afflicting only the female gender from the elderly age group, as the cases in this review ranged in age from 55 to 80 years (mean 66.6±8.55 years). On the other hand, dermal cylindromas (DC) are relatively prevalent benign skin adnexal tumours that often appear around the sixth decade of life as solitary or multiple lesions, with a male preponderance of 1:9 [1].
Histopathology has an important role in definitive diagnosis, and if achieved by core biopsy, a major surgical operation can be avoided. Accordingly, wide excision, excision biopsy, lumpectomy, and quadrantectomy were undertaken as curative options in 9 (90%) of the cases. There was one case by Liu et al. [10], in which radical mastectomy was undertaken because imaging had scored the lump high (BI-RADS ٤‒5) and core biopsy had documented occasional mitosis, leading to a diagnostic dilemma. The patient, however, had an uneventful follow-up period with no recurrence at 2 years. Otherwise also, none of the cases had any recurrence, supporting the benign nature of cylindroma.
In a study comparing breast cylindromas with dermal cylindromas and adenoid cystic breast carcinomas, Albores-Saavedra et al. [1] discovered that, with the exception of a slight increase in the quantity of eccrine ducts and reactive Langerhans cells in dermal cylindromas, the histologic and immunohistochemical characteristics of breast and dermal cylindromas were identical. Both were distinguished by epithelial islands with periphery myoepithelial cells and central basaloid cells encircled by a thicker, continuous, periodic acid-Schiff-positive basement membrane that was collagen IV immunoreactive. Breast cylindromas are characterized by clusters of sebaceous cells and a few eccrine ducts. Smooth muscle actin identified the peripheral myoepithelial cells in breast and dermal cylindromas, while cytokeratin-7 primarily labelled the central basaloid cells. Skin and breast cylindromas did not express estrogen receptors (ER) or progesterone receptors (PR), cytokeratin 20, or gross cystic disease fluid protein (GCDFP 15). In our study, we found a similar pattern in histopathology and immunochemistry analysis.
Establishing the diagnosis of CB is not particularly challenging but it is possible that a smaller sample of the lesion, such as a needle core biopsy, can be potentially misdiagnosed as a basaloid-appearing primary breast neoplasm with a differential diagnosis including adenoid cystic carcinoma, basaloid forms of ductal carcinoma-in-situ (DCIS), and solid/nested invasive ductal carcinoma [1, 11].
Solid variant of adenoid cystic carcinoma (ACC) is a particularly important differential since it shares the nodular and trabecular patterns, eccrine ducts, basaloid cells, myoepithelial cells, and hyaline globules of the basement membrane (BM). However, unlike BC, ACC has poor prognosis, lacks the continuous, thickened BM and displays cytologic atypia, mitotic figures and infiltrative growth pattern [11]. In rare situations where diagnosis is uncertain after histopathological analysis, molecular analyses can potentially aid in the differentiation between BC, which displays MYB expression and CYLD gene mutations, and ACC, with the characteristic presence of the MYB-NFIB fusion gene and MYB overexpression [14].
In our review, the 66-year-old-female presented by Fusco et al. [14] underwent right breast quadrantectomy with axillary sentinel lymph node excision after the screening mammography revealed an irregular dense shadow that was reported as ACC on core biopsy. After an uneventful recovery followed by absence of recurrence at 3 years, the diagnosis was BC was established after re-evaluation of biopsy specimen along with molecular studies including fluorescence in situ hybridization (FISH), reverse transcription PCR, immunohistochemistry and whole-exome sequencing, revealed an absence of the MYB-NFIB fusion gene, diminished levels of MYB protein expression and a clonal somatic CYLD splice site mutation associated with loss of heterozygosity of the wild-type allele. Escher-Michlig et al. [9] also detected the pathognomonic mutation of the CYLD gene mutation by whole exome sequencing in the specimen of BC excised in a 60-year-old female.
The fact that 5 (50%) of the cases had a history of cancer, either in the self (n = 3; 30%) or in the family (n = 2; 20%), is a significant finding from our review. The tumours (n = 2; 20%) were either solitary or multiple in type and included skin/anus squamous cell cancer, breast cancer, renal cancer, and colon cancer. This trend needs more research because it seems to point to a hereditary predisposition.
Conclusion
Cylindroma of the breast is a rare benign lesion found in elderly females and only ten cases could be identified in the English peer-reviewed literature during the 2016–2025 time frame. It should be kept in mind as a pitfall and a possible diagnosis when dealing with triple-negative breast tumours or the solid basaloid variant of adenoid cystic carcinoma in order to avoid overtreatment. Cylindroma has characteristic histopathological features and a molecular profile. Local excision is curative, and prognosis is excellent.
Contribution of the authors. Both the authors have participated in conception, data analysis and drafting of the manuscript and have approved the final manuscript.
Financial support and sponsorship. This project is entirely academic and non-commercial in nature, and it has neither sponsorship nor financial support.
Conflicts of interest. There are no conflicts of interest.
Data availability. Data can be obtained from the corresponding author upon request for a maximum of one year after the article’s publication.
Abbreviations
ACC ‒ adenoid cystic carcinoma;
BI-RADS ‒ Breast Imaging Reporting and Data System;
CB ‒ cylindroma of the breast;
DC ‒ dermal cylindroma;
DCIS ‒ ductal carcinoma in situ;
ER ‒ oestrogen receptor;
FISH ‒ fluorescence in situ hybridization;
GCDFP ‒ gross cystic disease fluid protein;
PR ‒ progesterone receptor.
References
1. Albores-Saavedra J, Heard SC, McLaren B, Kamino H, Witkiewicz AK. Cylindroma (dermal analog tumor) of the breast: a comparison with cylindroma of the skin and adenoid cystic carcinoma of the breast. Am J Clin Pathol 2005; 123(6): 866‒873. DOI: 10.1309/CRWU-A3K0-MPQH-QC4W.
2. Chauhan DS, Guruprasad Y. Dermal cylindroma of the scalp. Nat J Maxillofac Surg 2012; 3(1): 59–61. DOI: 10.4103/0975-5950.102163.
3. Singh DD, Naujoks C, Depprich R, Schulte KW, Jankowiak F, Kübler NR, Handschel J. Cylindroma of head and neck: review of the literature and report of two rare cases. J Craniomaxillofac Surg 2013; 41(6): 516–521.
4. Schwarz D, Drebber U, Ortmann M, Anagiotos A. Benign cylindroma: a rare differential diagnosis of external ear canal tumour. BMJ Case Rep 2016; 2016: bcr2015212035. DOI: 10.1136/bcr-2015-212035.
5. Gokaslan ST, Carlile B, Dudak M, Albores-Saavedra J. Solitary cylindroma (dermal analog tumor) of the breast: a previously undescribed neoplasm at this site. Am J Surg Pathol 2001; 25(6): 823–826. DOI: 10.1097/00000478-200106000-00017.
6. Papaoikonomou A, Chlorou A, Michailidou E, Panselinas G, Michailidi ME. Cylindroma of the breast: case report of a rare breast neoplasm. Cureus 2024; 16(9): e69896. DOI: 10.7759/cureus.69896.
7. McGhee K, Spethman C, Muhammad H, Woodard S, Guo H, Yalniz C. Breast cylindroma: a rare and unexpected diagnosis. Radiol Case Rep 2024; 19(11): 5144‒5148. DOI: 10.1016/j.radcr.2024.07.175.
8. Steinwehr D, Ghosh T, Bouton M. Cylindroma of the breast: a rare differential for breast cancer on core biopsies, case report and review of literature. J Investig Med High Impact Case Rep 2024; 12: 23247096241246627. DOI: 10.1177/23247096241246627.
9. Escher-Michlig V, Vlajnic T, Roma L, Marinucci M, Piscuoglio S, Matter M, Haug M, Weber WP, Muenst S. Cylindroma of the breast with CYLD gene mutation: a case report and review of the literature. Mol Biol Rep 2023; 50(8): 7133‒7139. DOI: 10.1007/s11033-023-08606-y.
10. Liu H, Wei C, Ding H, Zhang H. Primary cylindroma of the breast with brisk mitosis: a case report and review of literature. Int J Surg Pathol 2023; 31(5): 702–707. DOI: 10.1177/10668969221117255.
11. Halima A, Pannunzio AM, Erstine EM, Ko JS, Bergfeld WF, Malaya RM, Frankel MB, Calhoun BC, Sturgis CD. Cutaneous adnexal cylindroma of breast: epithelial immunoreactivities for GATA-3, mammaglobin, and E-cadherin do not equate to a mammary ductal neoplasm. Case Rep Pathol 2018; 2018: 4039545. DOI: 10.1155/2018/4039545.
12. Ahmed A, Rahmatalla N, Abdul-Hameed Ahmed A, Salih Rahmatalla N. Cylindroma of the breast ‒ rare to find, difficult to diagnose: a report of two cases. Iraq Med J 2018; 64: 187‒192.
13. Patel RK, Barnard KJ, Taylor JR, Howard CA, Jennings WC. The challenge of distinguishing cylindroma of the breast from adenoid cystic carcinoma: a case report and review of this rare tumor. Arch Breast Cancer 2017; 4: 28‒31. DOI: 10.19187/abc.20174128-31.
14. Fusco N, Colombo PE, Martelotto LG, De Filippo MR, Piscuoglio S, Ng CK, Lim RS, Jacot W, Vincent-Salomon A, Reis-Filho JS, Weigelt B. Resolving quandaries: basaloid adenoid cystic carcinoma or breast cylindroma? The role of massively parallel sequencing. Histopathology 2016; 68(2): 262‒271. DOI: 10.1111/his.12735.