Neurologijos seminarai ISSN ISSN 1392-3064 / eISSN 2424-5917
2024, 28(101), pp.207–213 DOI: https://doi.org/10.15388/NS.2024.28.101.7
Klinikinis atvejis / Case Reports
Ieva Lukauskaitė*
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
Jurgita Valaikienė
Vilnius University, Faculty of Medicine, Vilnius, Lithuania
Vilnius University, Faculty of Medicine, Institute of Clinical Medicine, Department of Neurology and Neurosurgery,
Vilnius, Lithuania
Summary. A 68-year-old male started experiencing a localized headache in the left temporal region, which later spread to the right side. Initially, his symptoms were nonspecific; therefore, he visited several neurologists and was diagnosed with cephalgia. However, the symptoms progressed, the pain spread to the temporomandibular joints, and problems with chewing and swallowing developed. One month later, the patient noticed a subfebrile fever, as well as a severe headache and swelling of the eyes; consequently, he was admitted to the Department of Internal Medicine. An increased erythrocyte sedimentation rate and C-reactive protein were established. Color-coded duplex sonography revealed the concentric hypoechoic thickness of the walls in both superficial temporal arteries with increased blood flow velocities. The temporal arteries were very rigid and painful; therefore, it was difficult to perform an ultrasound examination. Subsequently, giant cell arteritis was diagnosed. The patient received an intravenous course of methylprednisolone, followed by prednisolone and methotrexate tablets.
Five years later, the patient did not feel any pain or discomfort in the temporal area bilaterally at the follow-up visit. In control extracranial color-coded duplex sonography, the ‘halo’ sign was not observed, and the blood flow velocities were normal in both superficial temporal arteries. The ultrasound examination did not show signs of vasculitis.
Every patient aged >50 years old with a new onset of headache and an increased erythrocyte sedimentation rate of ≥ 50 mm/h and/or high C-reactive protein levels should be checked for giant cell arteritis. Patients with giant cell arteritis should be monitored closely not only to prevent relapses but also to evaluate complications of treatment. Color-coded duplex sonography of superficial temporal arteries is an advantageous method not only for diagnosis but also for the monitoring of the disease. Raising awareness of giant cell arteritis is paramount and can help diagnose it in time.
Keywords: giant cell arteritis, temporal arteritis, headache, ultrasound, color-coded duplex sonography.
Santrauka. 68 m. vyras susirgo palaipsniui – pajuto kairiojo smilkinio skausmą, kuris vėliau išplito į dešinę pusę. Pirminiai simptomai buvo nespecifiniai, todėl pacientui, kai apsilankė gydymo įstaigoje, buvo diagnozuota cefalgija, skirtas gydymas nuskausminamaisiais medikamentais. Bet simptomai progresavo, skausmas išplito į temporomandibuliarinį sąnarį, išsivystė kramtymo ir rijimo sutrikimai. Po mėnesio atsirado subfebrilus karščiavimas, stiprus galvos skausmas, patinimas apie akis, todėl pacientas buvo hospitalizuotas vidaus ligų skyriuje. Nustatyti padidėję uždegiminiai rodikliai. Spalvinės smilkinių duplekssonografijos metu buvo matomi koncentriniai hipoechogeniški abiejų paviršinių smilkininių arterijų sienelių sustorėjimai, registruoti padidėję kraujo tėkmės greičiai. Ultragarsinį tyrimą atlikti buvo sudėtinga, nes temporalinės arterijos buvo itin sukietėjusios ir skausmingos. Pacientui buvo diagnozuotas gigantinių ląstelių arteritas. Jis buvo gydomas intraveniniu metilprednizolono kursu, vėliau – peroraliniu prednizolonu ir metotreksatu.
Po penkerių metų, kontrolinio vizito metu, pacientas nebesiskundė nei galvos, nei žandikaulio skausmais. Spalvinės smilkinių sonoskopijos metu nebuvo matyti halo požymio, kraujo tėkmės greičiai abiejose paviršinėse temporalinėse arterijose buvo normalūs.
Vyresni nei 50 metų ligoniai, kuriems naujai atsiradęs galvos skausmas ar (ir) padidėjęs eritrocitų nusėdimo greitis ( ≥ 50 mm/val.) ir (ar) padidėjusi C reaktyvaus baltymo koncentracija, turėtų būti tiriami dėl gigantinių ląstelių arterito. Svarbu stebėti ligos eigą ne tik siekiant išvengti pasikartojimo epizodų, bet ir vertinant galbūt gydymo prednizolonu sukeltas komplikacijas. Smilkininių arterijų echoskopinis tyrimas yra tinkamas ne tik gigantinių ląstelių arterito pirminės diagnostikos, bet ir ligos monitoravimo metodas. Svarbu skleisti informaciją apie šią ligą, nes tai gali padėti laiku diagnozuoti šį vaskulitą ir išvengti sunkių komplikacijų.
Raktažodžiai: gigantinių ląstelių arteritas, temporalinis arteritas, galvos skausmas, ultragarsas, spalvinė duplekssonografija.
_________
* Address: Ieva Lukauskaitė, Čiurlionio 21, LT-03101 Vilnius, Lithuania. E-mail: ieva.lukauskaite@mf.stud.vu.lt. Mobile: + 370 626 65 710
Received: 05/01/2025. Accepted: 26/01/2025
Copyright © Ieva Lukauskaitė, Jurgita Valaikienė, 2024. Published by Vilnius University Press.This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Giant cell arteritis (GCA) is also known as temporal arteritis or Horton disease. GCA is the most common systemic vasculitis. It affects large and medium-sized arteries, especially the extracranial branches of the carotid artery. Accordingly, it causes a variety of neurological and ophthalmological complications [1]. In the past decades, superficial temporal artery biopsy was considered a gold standard for diagnosing GCA. However, due to its invasive nature and the significant number of false negative supplements, the importance of color-coded duplex sonography of superficial temporal arteries has been increasing. This diagnostic method is non-invasive and quick; therefore, it is currently of paramount importance in the initial diagnosis of GCA, as well as a controlling response to the therapy and monitoring for relapses. This clinical case illustrates the challenges and obstacles in diagnosing GCA, as well as the importance of color-coded duplex sonography in diagnosing and monitoring temporal arteritis.
A 68-year-old male started feeling a localized headache in the left temporal area, which later spread to the right side and occipital regions. Initially, his symptoms were nonspecific; therefore, he visited several neurologists, and brain magnetic resonance imaging (MRI) was performed, which revealed no lesions. In the laboratory tests, the inflammatory values were increased, C-reactive protein (CRP) was 70.59 mg/l, and the erythrocyte sedimentation rate (ESR) was 38 mm/h. Due to the unspecific manifestation of symptoms, borderline values of ESR and the absence of acute pathology visible on the brain MRI, he was diagnosed with cephalgia and received analgesic medication.
The patient also consulted an ophthalmologist and was diagnosed with presbyopia without further treatment recommended.
However, despite the analgetic treatment, the symptoms progressed, the pain started to spread to the temporomandibular joints, and problems with chewing and swallowing developed.
One month later, the patient noticed subfebrile fever up to 37.9° C, as well as a severe headache and periorbital swelling; consequently, he was admitted to the Department of Internal Medicine.
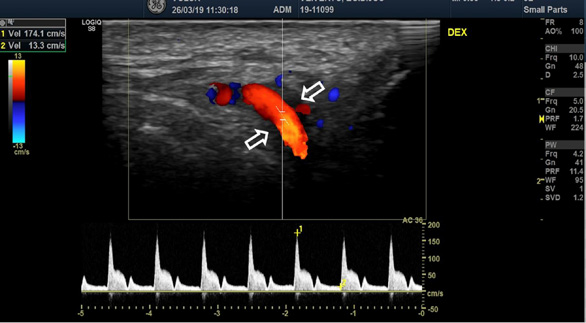
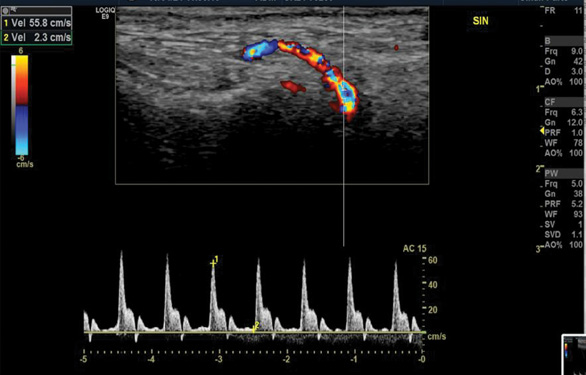
The blood test showed significantly increased CRP (208 mg/l), ESR (68 mm/h) and leucocytosis (12.30*10^9/l). Color-coded duplex sonography revealed the concentric hypoechoic thickness of the walls in both superficial temporal arteries, known as the ‘halo’ sign, which is a specific ultrasound finding in the case of GCA. The blood flow velocities of the superficial temporal artery were increased by approximately 200 cm/s bilaterally (Fig. 1 A, B).
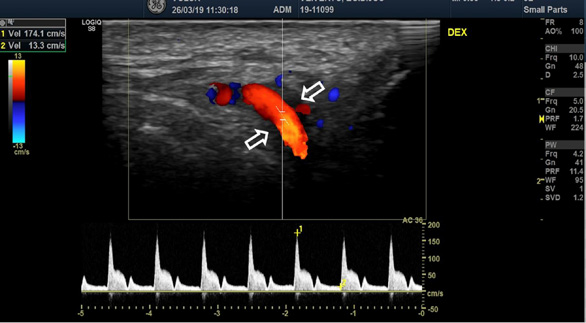
A
B
Color-coded duplex sonography revealed the typical ultrasound findings of temporal arteritis: the ‘halo sign’ as the dark area around the superficial temporal artery lumen probably due to arterial wall oedema (white arrows) with increased blood flow velocities on the right (A) and left (B) sides.
The temporal arteries were very rigid, with skin redness (Fig. 2) and painfulness, and therefore it was difficult to perform an ultrasound examination.

Inflammatory signs of the temporal arteries (skin redness, swelling, tenderness, painfulness, an elevated local temperature) were expressed.
GCA was diagnosed according to the American College of Rheumatologists and the European Alliance of Associations for Rheumatology (EULAR) criteria [2]. In the presented case, the patient scored a total of 16 points: 2 points for jaw claudication, 2 points for new-onset headache in the temporal region, 2 points for scalp tenderness and 2 points for abnormal scalp examination, 3 points for increased inflammation markers in the blood test (increased ESR and CRP), 5 points for the ‘halo’ sign in the sonography of the superficial temporal arteries.
The patient received an intravenous course of methylprednisolone, followed by prednisolone and methotrexate tablets. One week following the treatment, the control sonography was performed, which indicated a reduced ‘halo’ sign and reduced blood flow velocities bilaterally, thus showing the effectiveness of the treatment.
After starting treatment with corticosteroids, an elevated glucose level was detected. An endocrinologist consulted the patient. Glycemia values ranged from normal to 12.4 mmol/l, yet glycated haemoglobin values were consistent with those associated with type 2 diabetes. Therefore, type 2 diabetes was diagnosed, and treatment with metformin and insulin, as well as lifestyle changes, were recommended.
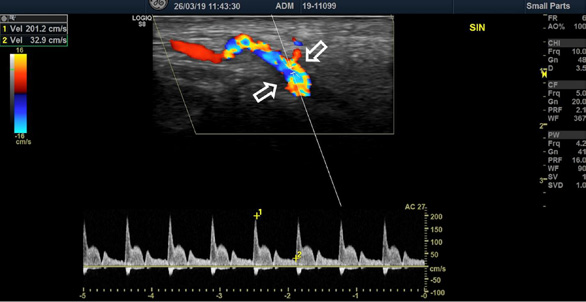
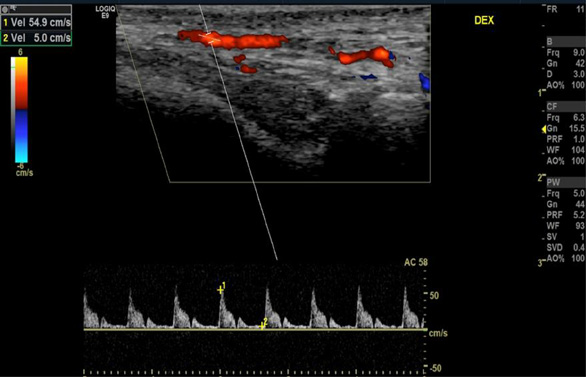
Five years later, at the follow-up visit, the patient did not feel any pain or discomfort in the temporal area bilaterally. No inflammatory signs of temporal arteries were detected (Fig. 3). The control color-coded duplex sonography showed no halo sign, and normal blood flow velocities were registered (Fig. 4). It was concluded that there were no clinical or ultrasound signs of temporal vasculitis.

A
B
The diabetes, which was a treatment complication, was well-controlled with the diet and appropriate physical activity.
No inflammatory signs of the temporal arteries were observed.
Normal blood flow velocities of the right (A) and left (B) superficial temporal arteries were observed without the ‘halo’ sign.
The clinical case shows that GCA can present with non-specific constitutional symptoms such as fatigue, fever, and muscle pain. In rare cases, the inflammatory markers of vasculitis can be within the normal range [3]. It is essential to suspect GCA, even when only constitutional symptoms are present in a patient over 50 years of age because, if not treated correctly, 15–20% of patients with GCA experience a vision loss in one eye; GCA also accounts for the majority of cases of tongue necrosis and can lead to other severe complications. [4]
Regarding diagnostic tests for GCA, color-coded duplex sonography of superficial temporal arteries is extremely important. The hallmark of vasculitis is a ‘halo’ sign, a hypoechoic noncompressible thickening of the wall in a temporal branch of the extracranial external carotid artery [5].
GCA is diagnosed according to the year 2022 EULAR and American College of Rheumatology criteria [2]. The mandatory criterion is the age of onset over 50 years old. The diagnostic clinical criteria are acute vision loss, a new onset temporal headache, scalp tenderness, jaw or tongue claudication, and neck or shoulder stiffness in the mornings. The laboratory, imaging and biopsy criteria are the following: an increased ESR (³50mm/h) and CRP concentration (³10mg/l2), positive superficial temporal artery biopsy or the ‘halo’ sign in color-coded duplex sonography of superficial temporal arteries, bilateral axillary involvement, FDG-PET activity throughout bilateral axillary involvement, FDG-PET activity throughout the aorta and its branches.
Temporal artery biopsy is considered a golden standard for diagnosing GCA. It has a low rate of complications (0.5%). In rare cases, it can even help differentiate GCA from ANCA-associated vasculitis or amyloidosis. However, it requires a highly experienced surgeon, as well as patient preparation for the surgical procedure in the head area and, in rare cases, can even lead to complications such as facial nerve palsy or scalp necrosis [6].
Color-coded duplex sonography of superficial temporal arteries is very beneficial when diagnosing GCA quickly to avoid complications such as permanent blindness. The superficial temporal arteries are only 4 mm below the skin; therefore, they offer excellent accessibility for ultrasound examination with very precise findings.
However, the swelling of the artery wall disappears within 2 or 3 weeks of treatment with corticosteroids, and the sonography may be uninformative. Therefore, knowing if the patient has already started corticosteroid treatment is very important [7].
Moreover, paradigmatic changes in GCA diagnostics have occurred; ultrasound has a benefit over temporal artery biopsy because it can be performed as a point-of-care test for fast-track diagnosis. It also has an emerging role in the monitoring of the disease. Significant sensitivity to changes in the ‘halo’ count was observed after the treatment initiation. Sonography is also an advantageous instrumental diagnostic method in diagnosing relapses of GCA. The ‘halo’ sign is present in most patients during the first relapse episode, although the number of segments with the ‘halo’ sign is lower [8].
Point-of-care ultrasound (POCUS) for diagnosing GCA is of great importance because it is associated with a lower prevalence of ophthalmological complications, especially permanent vision loss [9,10]. Most recent research also shows that fast-track temporal artery sonography can not only diagnose GCA accurately but also diagnose additional cases which were not possible to prove with the temporal artery biopsy [11]. Even though ultrasound depends on the experience and skills of the performer, it is an alternative to temporal artery biopsy which is inexpensive, non-invasive, widely available and safe [12].
1) Every patient >50 years old with a new onset of headache and/or an increased erythrocyte sedimentation rate ≥ 50mm/h and/or high C-reactive protein levels should be checked for giant cell arteritis.
2) Patients with giant cell arteritis should be monitored closely to prevent relapses and evaluate possible complications of the treatment.
3) Color-coded duplex sonography of superficial temporal arteries is a beneficial method not only for the initial diagnosis, but also for monitoring the disease.
4) Raising awareness of giant cell arteritis is paramount and can help diagnose this issue in a timely manner.