
Neurologijos seminarai ISSN ISSN 1392-3064 / eISSN 2424-5917
2024, 28(102), pp. 245–254 DOI: https://doi.org/10.15388/NS.2024.28.102.4
Apžvalginis mokslinis straipsnis / Review Article
Ainas Beinakaraitis
Lithuanian University of Health Sciences, Faculty of Medicine, Vilnius, Lithuania
ainas.beinakaraitis@stud.lsmu.lt
Livija Sadauskaitė
Lithuanian University of Health Sciences, Faculty of Medicine, Vilnius, Lithuania
livija.sadauskaite@stud.lsmu.lt
Augustė Juknelytė-Spūdienė
Lithuanian University of Health Sciences, Department of Neurology, Vilnius, Lithuania
auguste.juknelyte@stud.lsmu.lt
Antanas Vaitkus*
Lithuanian University of Health Sciences, Department of Neurology, Vilnius, Lithuania
Antanas.Vaitkus@lsmu.lt
Abstract. Headache is one of the common conditions affecting people worldwide, with migraines and tension-type headaches being the most prevalent. Pregnancy introduces hormonal fluctuations, particularly increased estrogen levels, which can influence headache characteristics. This study aimed to assess changes in headache patterns among pregnant women.
A prospective survey was conducted at the Lithuanian University of Health Sciences Kaunas Clinics (LSMUL KK), involving 67 pregnant women who experienced headaches before or during pregnancy. The participants completed a questionnaire evaluating headache characteristics and the MIDAS (Migraine Disability Assessment) questionnaire to assess functional impairment. The data were analyzed by using statistical methods, including the χ² test, the Mann-Whitney test, and the Fisher’s exact test.
It was found that 77.6% of the participants experienced headaches during pregnancy, compared to 89.6% before pregnancy. Among women who had headaches both before and during pregnancy, 70.5% reported no change in severity, while 29.5% experienced either worsening or improvement. Pressing and pulsating headache types decreased by approximately 25% during pregnancy. Besides, in 27.2% of the respondents, headache was associated with a reduction of daily activity impairment, thereby suggesting a potential positive impact of hormonal changes.
These findings highlight the complex interaction between pregnancy-related hormonal changes and headaches. While a significant fraction of women experience headache relief, others develop new headaches or undergo symptom worsening. Further research with larger cohorts is needed to deepen our understanding of the impact of pregnancy on headache disorders.
Keywords: Migraine, headache, pregnancy, headache characteristics.
Santrauka. Galvos skausmas yra viena dažniausių sveikatos būklių, paveikiančių žmones visame pasaulyje, o migrena ir įtampos tipo galvos skausmai yra patys dažniausi. Nėštumas lemia hormonų svyravimus, ypač padidėja estrogeno lygis, kuris gali turėti įtakos galvos skausmo pobūdžiui. Šio tyrimo tikslas buvo įvertinti galvos skausmo pokyčius nėštumo metu.
Lietuvos sveikatos mokslų universiteto ligoninėje Kauno klinikos (LSMUL KK) buvo atliktas perspektyvusis tyrimas, kuriame dalyvavo 67 nėščios moterys, patyrusios galvos skausmus prieš nėštumą arba jo metu. Dalyvės užpildė klausimyną, vertinantį galvos skausmo ypatumus, ir Migrenos sukeliamos negalios įvertinimo klausimyną (MIDAS), skirtą funkcinio sutrikimo analizei. Surinkti duomenys buvo analizuoti taikant statistinius metodus, įskaitant χ² testą, Manno–Whitney testą ir Fisherio tikslųjį testą.
Rezultatai parodė, kad galvos skausmus nėštumo metu patyrė 77,6 % moterų, palyginti su 89,6 % prieš nėštumą. Iš tų, kurios skundėsi galvos skausmais tiek prieš nėštumą, tiek jo metu, 70,5 % nepatyrė skausmo intensyvumo pokyčių, o 29,5 % teigė, kad skausmas arba sustiprėjo, arba susilpnėjo. Spaudžiantys ir pulsuojantys galvos skausmai nėštumo metu sumažėjo apie 25 %. Be to, 27,2 % respondenčių galvos skausmas buvo susijęs su sumažėjusiu kasdienių veiklų sutrikdymu, o tai leidžia manyti buvus galimą teigiamą hormoninių pokyčių poveikį.
Šie rezultatai parodo sudėtingą ryšį tarp nėštumo metu vykstančių hormonų pokyčių ir galvos skausmų. Nors nemažai daliai moterų skausmai susilpnėja, kitoms jie gali atsirasti pirmą kartą arba net pablogėti. Norint geriau suprasti nėštumo poveikį galvos skausmų pobūdžiui, būtini tolesni tyrimai sudarius didesnes tiriamųjų grupes.
Raktažodžiai: migrena, galvos skausmas, nėštumas, galvos skausmo ypatybės.
_______
* Address: Antanas Vaitkus, Lietuvos Sveikatos Mokslų Universitetas, Medicinos akademija, Medicinos fakultetas, Neurologijos klinika, Eivenių g. 2, Kaunas LT-50161. El. paštas antanas.vaitkus@kaunoklinikos.lt
Received: 28/04/2025. Accepted: 04/08/2025
Copyright © Ainas Beinakaraitis, Livija Sadauskaitė, Augustė Juknelytė-Spūdienė, Antanas Vaitkus, 2024. Published by Vilnius University Press.This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Headache is a persistent and relevant issue for people of all ages. Therefore, it is not surprising that every second person in the world and Europe experiences a headache at least once a year [1, 2]. It is evident from the scientific literature that, on any given day, up to 15.8% of people worldwide suffer from headaches [3, 4]. Headaches are classified into primary and secondary types. Primary headaches are not associated with any underlying disease, and headache is the only symptom experienced. Secondary headaches, on the other hand, are always linked to another pathology and are one of the symptoms of the underlying condition. Among primary headaches, migraine and tension-type headaches are the most common [5]. It is estimated that up to 40% of the population regularly experience tension-type headaches, and up to 15% suffer from migraines [1, 3, 5].
According to the Global Burden of Disease (GBD) 2019 study, the global prevalence of migraines has increased from 721.9 million to 833.4 million cases [6]. Individuals experiencing headaches lasting more than 15 days per month are classified as suffering from chronic migraine. It is known that up to 5% of the population suffer from chronic migraine, with women being more affected than men [5, 6]. Since migraines can occur frequently and persist for long periods, they rank as the second leading cause of disability for both genders and the primary cause among young women [4].
Among all headache disorders, migraines and tension-type headaches are most common during pregnancy. It is estimated that about 20% of women experience migraines during pregnancy [7, 8]. During pregnancy, hormonal concentrations change, which is believed to influence the characteristics of headaches [8, 9]. This change is associated with increased estrogen levels in the body. Estrogen is a pain-modulating hormone that affects various systems, including neurotransmitters such as serotonin and GABA, oxytocin, the trigeminovascular system, and the calcitonin gene-related peptide (CGRP) [10, 11, 12, 13].
Thus, headache patterns may change unpredictably. The objective of this study is to evaluate the characteristics and nature of headache changes in reproductive-age women during pregnancy.
The study was conducted with the approval of the Kaunas Regional Biomedical Research Ethics Committee (BE-2-78). It was carried out using a prospective method at the Hospital of the Lithuanian University of Health Sciences Kaunas Clinics (LSMUL KK).
A specially designed questionnaire was created for this study to assess changes in headaches experienced during pregnancy compared to those experienced before pregnancy. Only women who experienced headaches before or during pregnancy were included in the survey.
During the study, 67 pregnant women at LSMUL KK were surveyed about their headaches both before and during pregnancy. They were required to complete a questionnaire to evaluate the characteristics of their headaches. The participants answered questions regarding their headaches, their nature before pregnancy, and any changes during pregnancy. The MIDAS (Migraine Disability Assessment) questionnaire was used to assess the impact of headaches on daily activities during pregnancy.
The statistical analysis of the collected data was performed by using Microsoft Office Excel and IBM SPSS Statistics 29.0 software. The normality of the sample distribution was assessed using the Shapiro-Wilk test. The presentation of qualitative variables was achieved through the calculation of the frequency and relative frequency (in percentage terms) of the characteristics under study. The χ² test, the Mann-Whitney test, and the Fisher’s exact test were used for statistical analysis. Results were considered statistically significant when determining p < 0.05.
The study included 67 pregnant women. Demographic features of the participants are presented in Table 1.
|
Demographic feature |
Min |
Max |
Average |
Std. Deviation |
|
Age (years) |
21 |
42 |
32.69 |
5.100 |
|
Weight (kg) |
50 |
110 |
68.34 |
13.011 |
|
Pregnancy |
1 |
14 |
- |
- |
|
Trimester of pregnancy |
2 |
3 |
- |
- |
All surveyed women experienced migraines or tension headaches and had no secondary causes of headaches. Prior to pregnancy, 60 (89.6%) of the women reported experiencing headaches, while, during pregnancy, 52 (77.6%) of the women reported headaches. The majority of the participants, 44 women (65.7%), continued to experience headaches during pregnancy, whereas 8 (11.9%) developed headaches for the first time, and 15 (22.4%) no longer experienced headaches. It was determined that pregnancy does not statistically significantly influence the occurrence of headaches during pregnancy (p = 0.335).
Before pregnancy, 13 (21.6%) women reported mild headaches, 27 (45%) had moderate headaches, 16 (26.7%) experienced severe headaches, and 4 (6.7%) had unbearable headaches. During pregnancy, 8 (15.4%) women reported mild headaches, 27 (51.9%) had moderate headaches, 13 (25%) experienced severe headaches, and 4 (7.7%) suffered from unbearable headaches.
Among the 44 women who experienced headaches both before and during pregnancy, 31 (70.5%) reported no change in headache severity (of whom, 23 (52.3%) continued experiencing mild to moderate headaches, while 8 (18.2%) continued experiencing severe to unbearable headaches). However, 13 (29.5%) reported a change in headache severity (of whom, 5 (11.4%) worsened from mild/moderate to severe/unbearable, while 8 (18.2%) improved from severe/unbearable to mild/moderate levels). A statistically significant difference in headache severity before and during pregnancy was observed by using the Fisher’s exact test (p = 0.04).
Before pregnancy, 32 (53.3%) women reported headaches lasting up to 4 hours, 25 (41.7%) experienced headaches lasting between 4 and 72 hours, and 3 (5%) had headaches lasting longer than 72 hours. During pregnancy, 34 (65.4%) women experienced headaches lasting up to 4 hours, 16 (30.8%) had headaches lasting between 4 and 72 hours, and 2 (3.8%) had headaches lasting longer than 72 hours.
According to the MIDAS questionnaire, out of 52 women who experienced headaches during pregnancy 26 (50%) reported no disruption to daily activities, 14 (26.9%) experienced mild impairment, 9 (17.3%) had moderate impairment, whereas 3 (5.8%) reported severe impairment.
Changes in daily activities were evaluated among women who experienced headaches both before and during pregnancy. For 29 women, daily activities remained unchanged – of them, 9 had no impairment, while 20 continued to experience impairment. In 15 women, daily activity changes were observed: 12 no longer experienced impairment, while 3 developed new impairments. The impact of headaches on daily activities was therefore assessed, and it was found that headaches during pregnancy are statistically significantly less disruptive to daily activities compared to headaches prior to pregnancy (p = 0.042, Fisher’s exact test).
A comparison of headache characteristics before and during pregnancy is presented in Table 2.
|
Headaches Before Pregnancy |
||||||||
|
INTENSITY |
Count |
% |
DURATION |
Count |
% |
DAILY ACTIVITIES |
Count |
% |
|
Mild |
13 |
21.67% |
Lasts up to 4h |
32 |
53.33% |
Unaffected |
16 |
26.67% |
|
Moderate |
27 |
45.00% |
4-72h |
25 |
41.67% |
Affected |
44 |
73.33% |
|
Severe |
16 |
26.67% |
Over 72h |
3 |
5.00% |
|||
|
Unbearable |
4 |
6.67% |
||||||
|
Headaches During Pregnancy |
||||||||
|
INTENSITY |
Count |
% |
DURATION |
Count |
% |
DAILY ACTIVITIES |
Count |
% |
|
Mild |
8 |
15.38% |
Lasts up to 4h |
34 |
65.38% |
Unaffected |
26 |
50.00% |
|
Moderate |
27 |
51.92% |
4-72h |
16 |
30.77% |
Mild disruption |
14 |
26.92% |
|
Severe |
13 |
25.00% |
Over 72h |
2 |
3.85% |
Moderate disruption |
9 |
17.31% |
|
Unbearable |
4 |
7.69% |
Severe disruption |
3 |
5.77% |
|||
Pain localization did not differ significantly between pre-pregnancy and pregnancy periods. However, a notable decrease in unilateral headaches and an increase in whole-head headaches were observed during pregnancy. The most affected area was the temples, reported by approximately 35% of women both before and during pregnancy (see Figure 1).

Figure 1. Headache localization
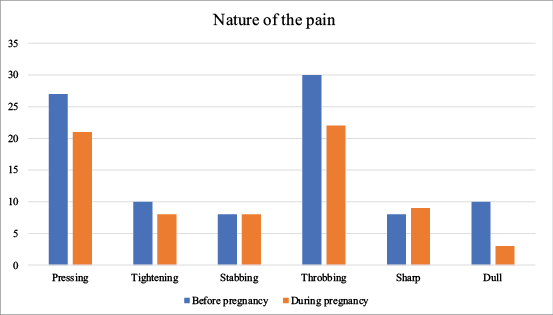
The nature of the pain slightly changed during pregnancy: pressing, pulsating, and dull headaches were less frequently reported in comparison to pre-pregnancy. Pressing and pulsating headaches decreased by approximately 25%, with their prevalence dropping to just over 20% during pregnancy. The prevalence of the nature of the pain is presented in Figure 2.
The most common headache-triggering factors among pregnant women were fatigue 30 (57.7%), stress 22 (42.3%), and insomnia 18 (34.6%).
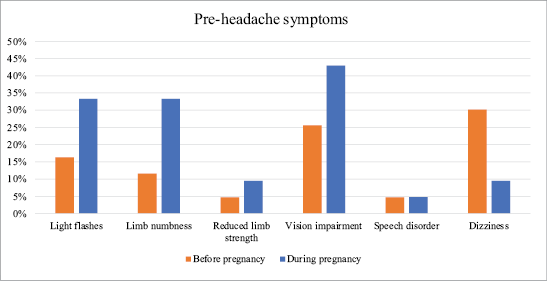
During pregnancy, most women reported experiencing visual disturbances (33.3%), flashes of light (33.3%), and limb numbness (42.9%) in addition to headache. A comparison indicated that relatively more women experienced pre-headache symptoms during pregnancy than before pregnancy (see Figure 3).
It was found that 18 (26.9%) women had been diagnosed with migraines. Among them, 7 (38.9%) experienced mild or moderate migraines before pregnancy, while 11 (61.1%) suffered from severe or unbearable migraines. For 8 (44.4%) of them during pregnancy, the intensity of their migraines remained unchanged, while, for 9 (50%), migraines decreased in severity or disappeared entirely, and only 1 (5.6%) case of an increase in severity was observed. Nevertheless, there is no statistically significant difference in migraine severity before and during pregnancy among migraineurs (p = 0.559).
Only 13 (19.4%) women, diagnosed with migraines, suffered from migraine during pregnancy. Among them, 7 (53.8%) experienced mild or moderate migraines during pregnancy, while 6 (46.2%) suffered from severe or unbearable migraines. The duration of migraines remained unchanged for 9 (69.2%), while 4 (30.8%) reported changes (2 (15.4%) experienced shorter durations, and 2 (15.4%) experienced longer durations). Hence, there is no statistically significant difference in the duration of migraines before and during pregnancy among migraineurs (p = 0.286). Due to migraines, 8 (61.5%) women continued to experience disruptions in daily activities, while 5 (38.5%) reported no longer being affected in this way.
Furthermore, the analysis also showed that women with migraines experienced significantly stronger headaches before pregnancy than those without migraines (p = 0.003). However, no statistically significant difference in headache severity, the duration of headaches (p = 0.419) or the impact on daily activities (p = 0.361) during pregnancy was found.
Epidemiological studies (Allais G. et al. (2018); Nam K.W. et al. (2023)) suggest that migraine symptoms improve in 60–70% of pregnant patients [10, 11]. Our study showed that headaches change during pregnancy compared to non-pregnancy periods, although statistically significant differences were rarely observed. This finding may be observed because the influence of hormones on headaches is not solely a pregnancy-related issue. Women often associate migraines with menstruation [10, 12, 13, 14]. Additionally, it has been noted that migraine attacks are linked to the use of hormonal contraceptives and hormone replacement therapy [10, 12, 13]. It is reasonable to hypothesize that estrogen is the most significant factor in this instance, as it has a protective effect against headaches by influencing various body systems. It alters the activity of neurotransmitters such as serotonin and GABA. An increase in estrogen leads to higher serotonin and GABA levels, which suppress pain [15]. Its effect on oxytocin also reduces pain perception [10, 12, 13, 15]. Additionally, its influence on the trigeminovascular system causes vasodilation and reduces the risk of migraines [12, 13, 16]. Therefore, estrogen fluctuations likely play a crucial role in modulating headache patterns during different periods in a woman’s life.
It is known that as pregnancy progresses, the duration, frequency, and intensity of headaches change, and sometimes even the nature of the headaches may vary [17, 18]. Studies (Raffaelli B. et al. (2017); Güzin Kardeş et al. (2023)) indicate that changes in headache characteristics occur in up to 86% of cases [17, 18]. The most common changes include headache intensity, location, and duration [17, 18]. Negro et al. (2017) observed that nearly two-thirds of patients experiencing primary headaches report less intense headaches or complete remission of symptoms [19]. In this study, most women did not experience significant changes in headache intensity or location. However, a difference in intensity was observed between non-pregnant and pregnant women. The most noticeable change was in the headache type, as pressing and pulsating headaches decreased by up to 25%, thereby suggesting a reduction in migraine prevalence. Nevertheless, this study demonstrates that, among migraineurs, there was no statistically significant difference in headache severity or the duration of headaches during pregnancy. Therefore, based on previous publications, the improvement or disappearance of migraines during pregnancy was not confirmed in this study [17, 18].
It was also found that symptoms preceding headaches change during pregnancy. Raffaelli B. et al. (2017) observed that up to 38.6% of women experience different pre-headache symptoms during pregnancy compared to before pregnancy [17]. It is estimated that up to 20% of women with migraine without aura may develop aura during pregnancy, while up to 14% of women with migraine with aura may experience its disappearance [19, 20]. In this study, relatively fewer women experienced pre-headache symptoms during pregnancy compared to non-pregnant women.
Pregnancy can also be associated with de novo cases of primary headaches, occurring in up to 5% of cases [10, 11, 21, 22]. The most reported new-onset headache type is migraine with aura [10, 13, 20]. In this study, new-onset headaches were much less common than headache remissions. However, none of the new headache cases in this study were associated with aura.
It has been demonstrated that pregnancy can result in the remission of headaches, the onset of new headaches, and alterations in the characteristics of existing headaches. However, the prevalence of these alterations can vary significantly.
It is of importance to note that headaches can disrupt daily activities. According to Ahmed (2012) and Mathew (2001), up to 81% of women experiencing headaches report some level of functional impairment [23, 24]. Our study yielded similar results, with 26.87% of women reporting no impairment in daily activities. Additionally, 34.33% of women in our study experienced reduced or eliminated daily activity disruptions, likely due to a decreased headache intensity. Only 8.96% of women reported new daily activity impairment, which may be explained by the limited treatment options available during pregnancy [14, 19].
There are few studies on headaches in pregnancy worldwide, and little to none in Lithuania. Studying headaches is valuable due to potential health risks involved. Pregnancy-related complications (preterm birth, gestational hypertension, preeclampsia) are associated with headaches [17, 25, 26, 27]. Headaches are also linked to up to a twofold increased risk of cardiovascular diseases, which can lead to complications [10, 11, 28]. It is estimated that up to 50% of women with headaches may experience adverse pregnancy outcomes [19, 29]. Therefore, secondary headache causes must first be ruled out. In this study, we did not analyze women with secondary headaches, however, primary headaches occur more frequently than secondary headaches, thus making it essential to identify primary headaches, particularly since there is a lack of research on their characteristics during pregnancy [17, 20, 26, 30, 31].
One limitation of our study is the small sample size and the method of data collection, as the participants were only being surveyed in the obstetrics department. This led to another limitation – notably, that most women were surveyed during their third trimester. However, migraine is, actually, most experienced in the first trimester, with symptoms decreasing in the third trimester [29]. Additionally, secondary headaches become more prevalent in the third trimester compared to other pregnancy stages, which means that our data may fail to fully represent headaches experienced throughout pregnancy [27]. Due to the small sample size, further studies with larger cohorts and surveys conducted at different pregnancy stages are still required.
This study observed changes in headache characteristics among pregnant women. Most notably, 29.5% of the participants experienced changes in headache intensity, with intensity decreasing in 18.2% of cases. Additionally, the headache type changed, with pressing and pulsating headaches decreasing by 25% during pregnancy. It has also been found that migraine patients experienced more severe headaches before pregnancy than non-migraine patients. However, no other significant difference in headache features was observed between the two groups during pregnancy. Finally, it is noteworthy that 27.2% of the participants demonstrated a reduction in daily activity impairment. These findings showcase that hormonal changes during pregnancy can lead to both improvements and new challenges regarding headaches.